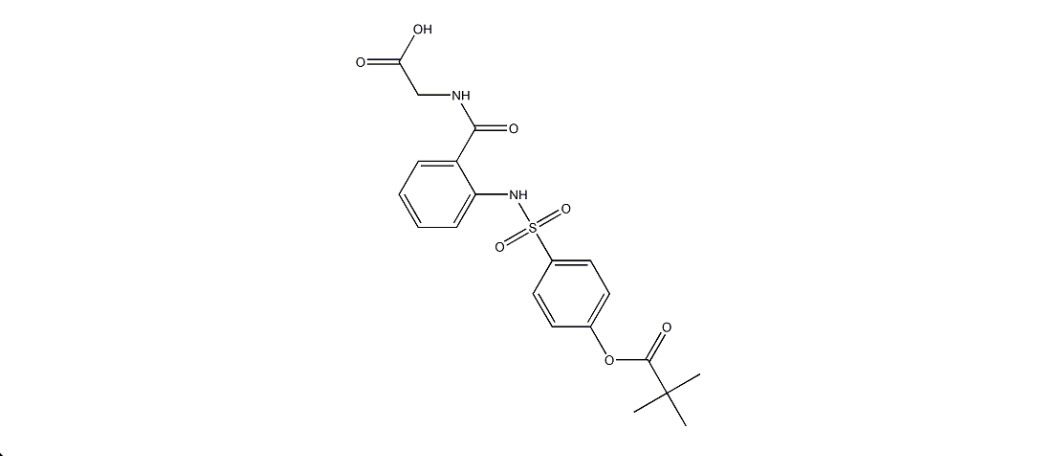
Adalimumab
Overview
Adalimumab is a fully human recombinant immunoglobulin G1 monoclonal antibody designed to specifically bind and neutralize tumor necrosis factor alpha, a key pro-inflammatory cytokine involved in immune-mediated inflammation. By inhibiting both soluble and membrane-bound forms of tumor necrosis factor alpha, adalimumab disrupts downstream inflammatory signaling pathways that contribute to tissue damage, pain, and disease progression. This targeted biological mechanism allows for effective control of chronic inflammation across a range of autoimmune and inflammatory disorders. Adalimumab is administered by subcutaneous injection and is suitable for long-term use under medical supervision. Its consistent immunomodulatory effect has made it a foundational therapy in rheumatology, gastroenterology, dermatology, and ophthalmology, where sustained suppression of pathological inflammation is required to improve symptoms and prevent disease complications.
Background and Date of Approval
Adalimumab was developed as the first fully human monoclonal antibody targeting tumor necrosis factor alpha, aiming to reduce immunogenicity associated with earlier biologic therapies. It received approval from the United States Food and Drug Administration in 2002 for the treatment of moderately to severely active rheumatoid arthritis. The European Medicines Agency granted approval in September 2003. Subsequent regulatory approvals expanded its indications to include multiple inflammatory conditions based on evidence from pivotal clinical trials demonstrating sustained efficacy and an acceptable safety profile. Over time, adalimumab became one of the most widely prescribed biologic therapies globally, with multiple biosimilar versions approved following the expiration of original patent protections.
Uses
Adalimumab is indicated for the treatment of several immune-mediated inflammatory diseases in adult and selected pediatric populations. Approved indications include rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, chronic plaque psoriasis, Crohn’s disease, ulcerative colitis, juvenile idiopathic arthritis in patients aged two years and older, hidradenitis suppurativa, and non-infectious uveitis. Depending on the condition and disease severity, adalimumab may be used as monotherapy or in combination with other disease-modifying treatments to achieve optimal disease control.
Administration
Adalimumab is administered via subcutaneous injection, commonly into the thigh or abdomen, with rotation of injection sites to minimize local skin reactions. Standard adult dosing for many indications involves administration every other week, though weekly dosing may be required in certain conditions or in cases of inadequate response. Some indications require initial loading doses followed by maintenance therapy. Pediatric dosing is weight-based. Dosing schedules are individualized according to the specific disease, patient response, and tolerability, with regular clinical review to guide adjustments.
Side Effects
Common side effects associated with adalimumab include injection site reactions such as pain, redness, swelling, or itching. Systemic effects may include upper respiratory tract infections, sinusitis, headache, fatigue, and rash. Gastrointestinal discomfort may also occur. These effects are generally mild to moderate in severity and often resolve with continued treatment or supportive care.
Warnings
Adalimumab carries important warnings for serious infections, including tuberculosis, invasive fungal infections, and other opportunistic infections that may be life-threatening. An increased risk of malignancies, including lymphoma and non-melanoma skin cancers, has been reported with tumor necrosis factor inhibitors. Reactivation of hepatitis B virus may occur in carriers. Other serious risks include worsening or new-onset congestive heart failure, demyelinating disorders, lupus-like syndromes, cytopenias, and severe hypersensitivity reactions. Live vaccines should generally be avoided during treatment.
Precautions
Before initiating adalimumab, patients should be screened for latent tuberculosis, hepatitis B infection, and other chronic infections. Baseline and periodic monitoring of blood counts and liver function is recommended. Concomitant use with other biologic immunosuppressants is generally avoided due to increased infection risk. Vaccination status should be reviewed prior to therapy initiation, and live vaccines should not be administered during treatment. Patients should be closely monitored for signs of infection or neurological symptoms throughout therapy.
Expert Tips
Appropriate patient selection and baseline screening are essential before starting adalimumab therapy. Educate patients on correct injection technique, proper storage, and recognition of early signs of infection. Regular follow-up should include assessment of disease activity, safety monitoring, and adherence. Prompt evaluation of unexplained fever, persistent cough, or unusual neurological symptoms is recommended. Coordination with specialists enhances treatment outcomes, particularly in patients receiving long-term biologic therapy.