Atezolizumab
Overview
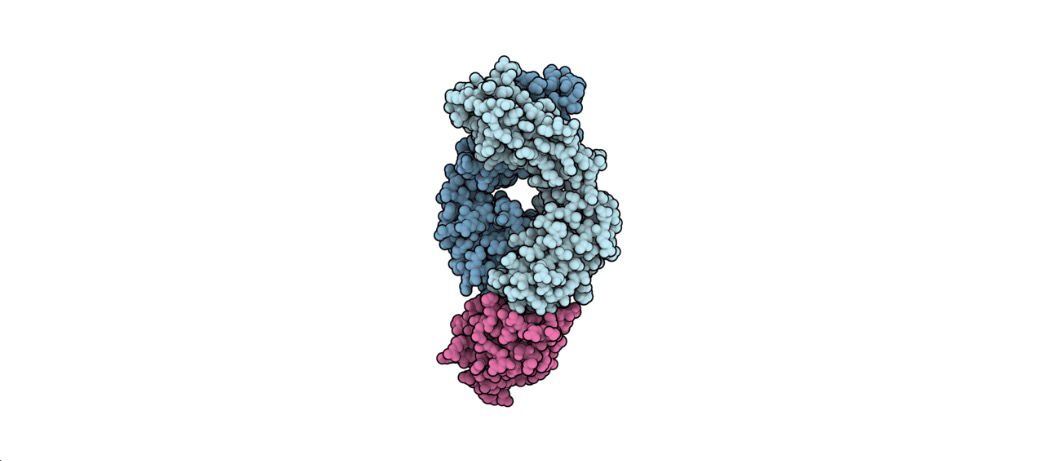
Atezolizumab is a humanized IgG1 monoclonal antibody that targets programmed cell death ligand 1 (PD-L1). By inhibiting PD-L1, it restores T-cell mediated immune responses against cancer cells, improving the body's ability to control tumor growth. Approved by the FDA in 2016, Atezolizumab is indicated for a range of cancers including non-small cell lung cancer (NSCLC), small cell lung cancer (SCLC), hepatocellular carcinoma (HCC), triple-negative breast cancer (TNBC), and alveolar soft part sarcoma (ASPS). The drug can be administered as monotherapy or in combination with chemotherapy or targeted therapy, depending on the tumor type and stage. Its mechanism of action, targeting the PD-1/PD-L1 immune checkpoint pathway, makes it a cornerstone of modern immuno-oncology treatments. Atezolizumab has demonstrated improved overall survival and durable responses in multiple clinical trials, establishing its role in both first-line and subsequent cancer therapy.
Background and Date of Approval
Atezolizumab was developed to overcome tumor immune evasion by blocking PD-L1 interaction with PD-1 and B7.1 receptors. The FDA granted accelerated approval for metastatic NSCLC in 2016 after clinical trials showed improved survival compared with standard chemotherapy. Subsequent approvals expanded to SCLC in combination with chemotherapy, HCC in combination with bevacizumab, TNBC with nab-paclitaxel, and rare cancers such as ASPS. Pivotal trials such as OAK and POPLAR demonstrated significant progression-free and overall survival benefits. EMA approval followed similar timelines, confirming the global recognition of Atezolizumab as a key immunotherapy. The development of Atezolizumab reflects the evolution of immune checkpoint inhibitors in oncology, providing patients with more targeted and effective treatment options.
Uses
Atezolizumab is indicated for multiple cancer types. In NSCLC, it is used as adjuvant therapy after resection and platinum-based chemotherapy in PD-L1 positive tumors, and as first-line therapy for metastatic disease in high PD-L1 expressers. In SCLC, Atezolizumab is combined with carboplatin and etoposide for extensive-stage disease. For HCC, it is used with bevacizumab for unresectable or metastatic cases without prior systemic therapy. In TNBC, the drug is combined with nab-paclitaxel for first-line treatment of PD-L1 positive metastatic disease. Atezolizumab is also approved for ASPS in adults and pediatric patients aged 2 years and older with unresectable or metastatic disease. This therapy is essential in HER2-negative tumors and provides durable responses in immunotherapy-sensitive malignancies.
Administration
Atezolizumab is administered intravenously, with dosing dependent on indication and patient factors. For most adult indications, a dose of 1200 mg is given every three weeks. For TNBC, dosing may be 840 mg every two weeks or 1200 mg every three weeks depending on chemotherapy combination. Infusions typically last 60 minutes for the first dose and can be reduced to 30 minutes for subsequent doses if tolerated. Therapy continues until disease progression or unacceptable toxicity in metastatic settings, or as specified in clinical protocols for adjuvant or neoadjuvant use. Close monitoring during infusion is required to manage potential reactions.
Side Effects
Common adverse reactions include fatigue, decreased appetite, nausea, cough, dyspnea, constipation, and musculoskeletal pain. Infusion-related reactions may occur, particularly during initial doses. These side effects are generally manageable with supportive care and do not necessitate therapy discontinuation in most cases. Patients should report persistent or worsening symptoms to their healthcare provider promptly.
Warnings
Serious immune-mediated events can occur, including pneumonitis, hepatitis, colitis, endocrinopathies, and nephritis. These can be life-threatening if not recognized and managed promptly. Cardiac, hepatic, and pulmonary monitoring is recommended during therapy. Atezolizumab can cause fetal harm if administered during pregnancy, and effective contraception is required for patients of childbearing potential. Severe infusion reactions and rare hypersensitivity events may also occur. Dose interruption or discontinuation is advised in cases of severe toxicity.
Precautions
Patients should be screened for pre-existing autoimmune conditions before therapy. Concomitant immunosuppressive medications may reduce efficacy or increase risk of adverse events. Careful consideration is required when combining with other therapies, and regular monitoring of liver function, thyroid function, and complete blood counts is recommended. Dose adjustments may be necessary for severe toxicity or organ dysfunction. Patient education on symptom reporting is essential for safe treatment.
Expert Tips
Clinicians should ensure accurate PD-L1 testing and confirm cancer type before initiating therapy. Regular monitoring of hepatic, pulmonary, and endocrine function is critical. Pharmacists should educate patients on recognizing early signs of immune-mediated adverse events and the importance of adhering to infusion schedules. Supportive care measures for fatigue, nausea, and other common side effects can improve patient adherence and treatment outcomes. Coordination with oncology nursing staff ensures proper infusion management and monitoring for infusion-related reactions.
