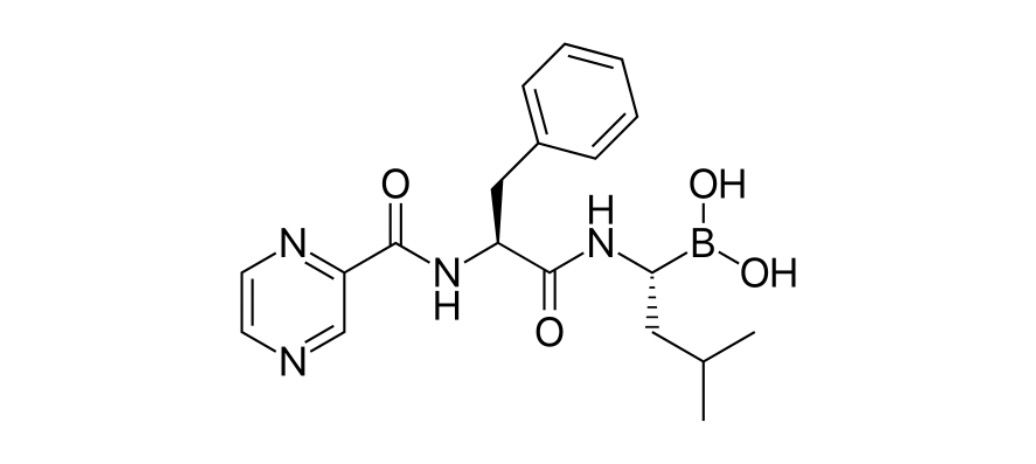
Bortezomib
Overview
Bortezomib is a targeted anticancer therapy classified as a proteasome inhibitor. It works by blocking the activity of proteasomes, which are cellular complexes that break down proteins. By inhibiting proteasomes, bortezomib causes an accumulation of proteins within cancer cells, leading to stress and cell death. This mechanism is particularly effective against plasma cells in multiple myeloma and malignant cells in mantle cell lymphoma.
Background and Date of Approval
Bortezomib was the first proteasome inhibitor to be approved for clinical use. It received approval from the U.S. Food and Drug Administration in 2003 for the treatment of relapsed and refractory multiple myeloma. Later, its use expanded to include mantle cell lymphoma and frontline therapy in combination regimens. The approval of bortezomib marked a significant breakthrough in oncology, providing new treatment options for patients with blood cancers and improving survival outcomes.
Uses
Bortezomib is primarily indicated for the treatment of multiple myeloma, either as a single agent or in combination with other medicines such as lenalidomide, thalidomide, melphalan, and dexamethasone. It is also approved for the treatment of mantle cell lymphoma in patients who have received at least one prior therapy. Research and clinical experience have demonstrated that bortezomib can be effective in improving progression-free survival and overall response rates in these conditions.
Administration
Bortezomib can be administered either as an intravenous injection or as a subcutaneous injection. The standard dosing schedule is usually twice weekly for two weeks followed by a rest period, although treatment regimens may vary based on the indication and whether bortezomib is used alone or in combination therapy. Proper hydration and supportive care are important during treatment to reduce side effects. The dosing is carefully adjusted depending on patient tolerability, blood counts, and organ function.
Side Effects
The most frequent side effects of bortezomib include fatigue, nausea, diarrhea, constipation, decreased appetite, low platelet counts, and peripheral neuropathy. Many patients experience mild to moderate gastrointestinal symptoms or temporary changes in blood counts, which are typically manageable with supportive care or dose adjustments.
Warnings
Serious risks of bortezomib include severe neuropathy, heart failure, pulmonary toxicity, liver injury, and severe cytopenias such as neutropenia and thrombocytopenia. Rare but significant risks include posterior reversible encephalopathy syndrome and tumor lysis syndrome. Infections may occur due to immune suppression, and antiviral prophylaxis is often recommended to prevent herpes zoster reactivation. Patients should be closely monitored throughout therapy with blood counts and organ function tests.
Precautions
Bortezomib should be used cautiously in patients with preexisting neuropathy, liver dysfunction, or heart disease. It is metabolized in the liver, and interactions may occur with drugs that affect cytochrome P450 enzymes. Concomitant use with strong CYP3A4 inducers or inhibitors should be carefully managed. Bortezomib should not be used during pregnancy, and effective contraception is required for both male and female patients of reproductive potential.
Expert Tips
Prescribers should tailor dosing schedules to minimize toxicity while maximizing response. Regular assessment of neuropathy symptoms is essential, and dose reductions may be required if symptoms worsen. Pharmacists should counsel patients about reporting numbness, tingling, or burning sensations early, as peripheral neuropathy can become irreversible. Patients should also be reminded to stay hydrated and maintain good nutritional support during therapy.
