Cabazitaxel
Overview
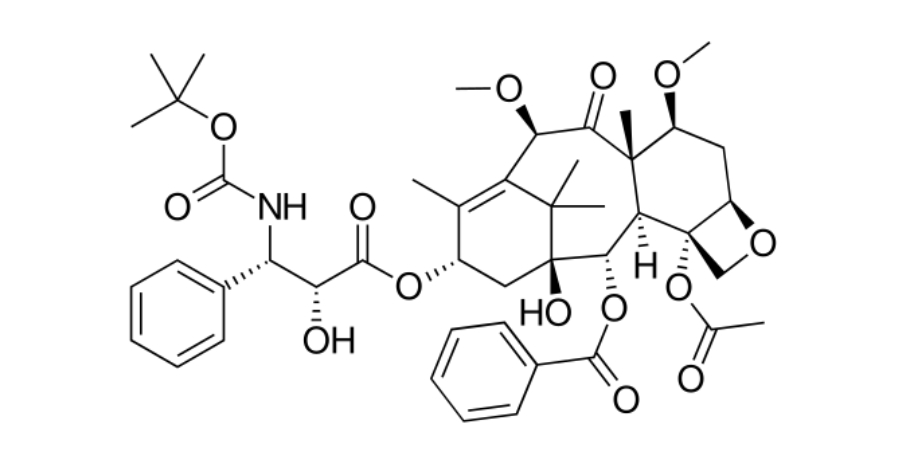
Cabazitaxel is a semi-synthetic taxane class antineoplastic chemotherapy agent used in the management of advanced prostate cancer. It works by binding to tubulin and stabilizing microtubules, which disrupts normal microtubule dynamics required for cell division and intracellular transport. This leads to cell cycle arrest and apoptosis of rapidly dividing cancer cells. Cabazitaxel is administered intravenously and is designed to retain activity in tumors that have developed resistance to earlier taxanes such as docetaxel. Its limited affinity for common drug efflux pumps contributes to its effectiveness in resistant disease. Clinically, cabazitaxel plays an important role in later-line treatment of metastatic castration-resistant prostate cancer, offering a survival benefit in patients who have progressed after standard chemotherapy. Due to its cytotoxic nature, treatment is delivered in specialized oncology settings with careful patient selection and monitoring. Cabazitaxel is typically combined with oral corticosteroids to support treatment tolerance and clinical outcomes.
Background and Date of Approval
Cabazitaxel was developed by Sanofi-Aventis as a next-generation taxane to address resistance seen with earlier agents. It received its first regulatory approval from the United States Food and Drug Administration in June 2010 for the treatment of metastatic castration-resistant prostate cancer in patients previously treated with docetaxel. The European Medicines Agency granted marketing authorisation for cabazitaxel in March 2011. Based on further clinical evidence demonstrating comparable survival outcomes with improved tolerability, a lower dose regimen of cabazitaxel received FDA approval on September 14, 2017. These approvals were supported primarily by the TROPIC phase III clinical trial program, which demonstrated a significant survival benefit in this patient population.
Uses
Cabazitaxel is indicated for the treatment of metastatic castration-resistant prostate cancer in adult patients whose disease has progressed during or after docetaxel-based chemotherapy. It is used in combination with oral prednisone or prednisolone. Cabazitaxel is generally reserved for patients requiring second-line or later systemic chemotherapy due to disease progression despite standard hormonal and chemotherapeutic treatments.
Administration
Cabazitaxel is administered as an intravenous infusion over approximately one hour in a controlled clinical environment. The standard recommended dose is 20 mg per square meter of body surface area given once every three weeks in combination with daily oral prednisone. In selected patients with adequate bone marrow reserve and clinical fitness, a higher dose of 25 mg per square meter may be considered with appropriate supportive care. Premedication with antihistamines, corticosteroids, and antiemetics is required prior to infusion to reduce the risk of hypersensitivity reactions. Treatment continues in cycles based on response, tolerance, and disease progression, with routine laboratory monitoring before each cycle.
Side Effects
Commonly observed side effects of cabazitaxel include neutropenia, anemia, leukopenia, thrombocytopenia, diarrhea, nausea, vomiting, constipation, fatigue, weakness, decreased appetite, peripheral neuropathy, back pain, fever, cough, shortness of breath, and changes in taste. The frequency and severity of these effects vary between patients and are generally manageable with appropriate medical supervision and supportive care.
Warnings
Serious adverse events associated with cabazitaxel include severe neutropenia, febrile neutropenia, serious infections, and sepsis, which can be life-threatening. Severe hypersensitivity reactions may occur during infusion and require immediate medical intervention. Significant gastrointestinal toxicity such as severe diarrhea, dehydration, and electrolyte imbalance has been reported. Cabazitaxel is contraindicated in patients with severe hepatic impairment and in those with critically low baseline neutrophil counts. The drug poses a risk of fetal harm and should not be used during pregnancy. Effective contraception is required for patients of reproductive potential during and after treatment.
Precautions
Baseline evaluation before initiating cabazitaxel should include complete blood counts and assessment of liver and renal function. Elderly patients may be at increased risk of toxicity and require closer monitoring. Cabazitaxel is metabolized primarily through hepatic CYP3A pathways, and caution is advised when used with strong CYP3A inhibitors or inducers. Live vaccines should generally be avoided during treatment due to immunosuppression. Although classical drug interactions are less common with intravenous chemotherapy, careful review of concomitant medications is essential.
Expert Tips
Appropriate patient selection for cabazitaxel includes confirmation of disease progression after docetaxel therapy and adequate bone marrow function. Baseline and ongoing monitoring should focus on blood counts, liver function, and early signs of infection or gastrointestinal toxicity. Patients should be counselled to report fever, persistent diarrhea, or symptoms suggestive of infection immediately. Strict adherence to corticosteroid co-therapy and premedication protocols is essential. Infusion preparation and administration should follow established cytotoxic handling guidelines, with readiness to manage hypersensitivity reactions. Coordination with supportive care measures such as growth factor support can improve treatment tolerability.
