Carfilzomib
Overview
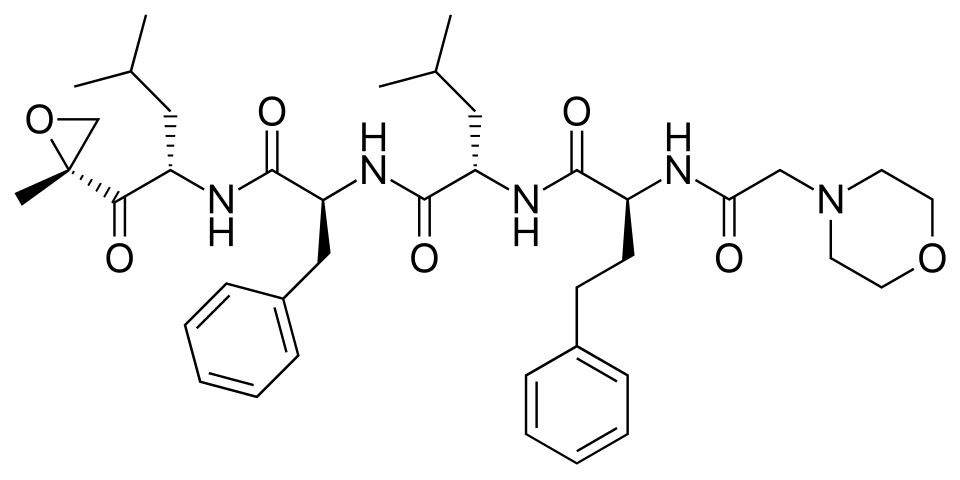
Carfilzomib is a second‑generation small‑molecule proteasome inhibitor that irreversibly binds to the chymotrypsin‑like active site of the 20S proteasome, leading to accumulation of unwanted intracellular proteins and triggering apoptotic cell death in malignant cells. This mechanism targets the proteasome pathway, which is essential for the degradation of misfolded and regulatory proteins, making carfilzomib effective in multiple myeloma cells that rely on high proteasome activity for survival. Carfilzomib’s targeted action distinguishes it from traditional cytotoxic chemotherapy by focusing on a cellular degradation pathway, thereby reducing tumor burden and inducing responses in patients with relapsed or refractory disease. The drug is administered intravenously under clinical supervision and is used either as monotherapy or in combination with standard antimyeloma agents such as dexamethasone, lenalidomide, or monoclonal antibodies depending on treatment history and protocol. Its role has expanded with additional combinations that further enhance therapeutic outcomes in later lines of therapy.
Background and Date of Approval
Carfilzomib, marketed under the brand name Kyprolis, received initial approval from the United States Food and Drug Administration in July 2012 for the treatment of adult patients with relapsed or refractory multiple myeloma who had previously received at least two lines of therapy including a proteasome inhibitor and an immunomodulatory agent. Additional supplemental approvals expanded its indications to include use in combination with dexamethasone or with lenalidomide and dexamethasone for patients who have received one to three prior lines of therapy, and later to include combinations with monoclonal antibodies such as daratumumab plus dexamethasone. Regulatory authorities outside the United States have similarly authorized carfilzomib for multiple myeloma in comparable clinical settings.
Uses
Carfilzomib is indicated for adult patients with relapsed or refractory multiple myeloma. It may be used as a single‑agent therapy for patients who have received one or more prior therapies or in combination with dexamethasone, with lenalidomide plus dexamethasone, or with monoclonal antibodies such as daratumumab plus dexamethasone, depending on the number of prior lines of therapy and clinical context. These combination regimens are designed to enhance response rates and prolong progression‑free survival in patients who have relapsed after initial treatments or whose disease is refractory to standard therapies.
Administration
Carfilzomib is administered by intravenous infusion under careful clinical supervision. Standard dosing regimens include weight‑based dosing on a body surface area basis, with typical schedules involving administration on two consecutive days per week for three weeks of a 28‑day cycle. Initial cycles often start at a lower dose with escalation in subsequent cycles if tolerated, depending on the specific combination regimen and protocol. Premedication with agents such as dexamethasone and adequate hydration are recommended to mitigate infusion‑related and renal risks. Baseline and periodic assessments of cardiac, renal, and hematologic function guide dose adjustments and treatment continuation.
Side Effects
Common side effects observed with carfilzomib include fatigue, anemia, thrombocytopenia, neutropenia, nausea, diarrhea, dyspnea, upper respiratory tract infection, hypertension, fever, cough, insomnia, and musculoskeletal pain. The incidence and severity of these effects vary among patients and may be influenced by concomitant therapies and disease burden. Many of these effects are manageable with supportive care, dose modifications, and symptomatic treatment under medical supervision.
Warnings
Serious adverse events associated with carfilzomib include cardiac toxicities such as new onset or worsening heart failure, myocardial ischemia, and myocardial infarction; acute renal failure; tumor lysis syndrome; pulmonary toxicity including acute respiratory distress syndrome; pulmonary hypertension; severe hypertension; and venous thromboembolism. Infusion reactions and rare neurologic syndromes such as posterior reversible encephalopathy syndrome have been reported. Carfilzomib can cause significant toxicity, and its use requires careful monitoring and management of these risks. It is contraindicated in patients with known hypersensitivity to carfilzomib.
Precautions
Before initiating carfilzomib, baseline assessments should include complete blood counts, cardiac evaluation, renal and liver function tests, and assessment of fluid status. Special caution is warranted in patients with pre‑existing cardiac disease, impaired renal function, pulmonary disorders, and significant hypertension. Adequate hydration and monitoring of electrolytes are recommended to reduce the risk of renal toxicity and tumor lysis syndrome. Concomitant use of other cardiotoxic agents should be carefully considered. Live vaccines should be avoided during significant immunosuppression. Regular clinical and laboratory monitoring is essential to detect toxicities early and guide therapeutic adjustments.
Expert Tips
Patient selection for carfilzomib therapy involves confirming a diagnosis of relapsed or refractory multiple myeloma and evaluating prior treatment history. Baseline and ongoing monitoring of cardiac function, blood pressure, renal function, and complete blood counts is critical to anticipating and managing toxicities. Patients should be counselled on recognizing symptoms of cardiac distress, infusion reactions, respiratory symptoms, and signs of infection. Premedication with corticosteroids and ensuring adequate hydration before each dose may reduce adverse events. Coordination with multidisciplinary oncology care teams ensures timely assessments, dose modifications, and supportive care interventions to optimize therapeutic outcomes and safety.
