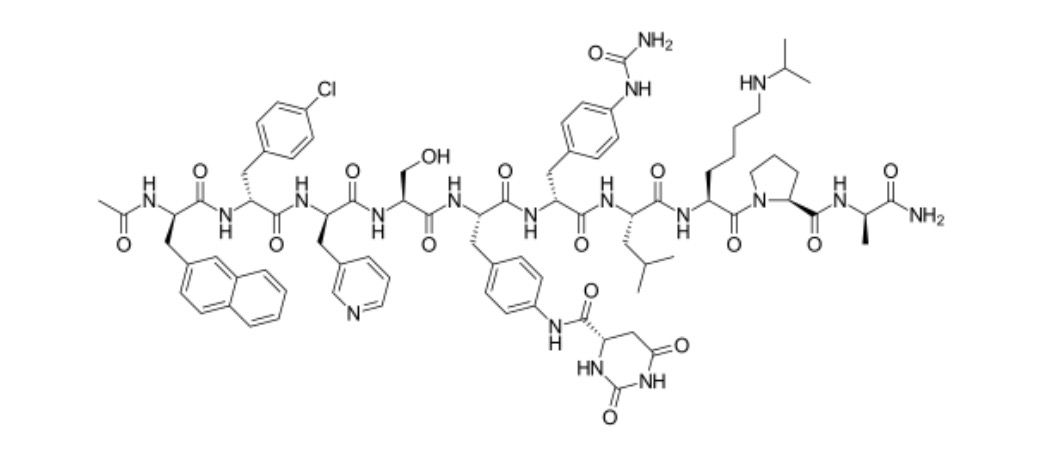
Degarelix
Overview
Degarelix is a synthetic peptide and a gonadotropin‑releasing hormone (GnRH) receptor antagonist that rapidly suppresses pituitary release of luteinizing hormone and follicle‑stimulating hormone, leading to a decrease in testosterone production by the testes. Its mechanism involves direct competitive blockade of GnRH receptors in the anterior pituitary, which differentiates it from GnRH agonists that can initially cause a surge in luteinizing hormone and testosterone before suppression. Because degarelix avoids this hormonal surge, it is used therapeutically to achieve rapid testosterone suppression without the transient increase in hormone levels that can worsen symptoms in hormone‑dependent prostate cancer. It is administered by subcutaneous injection and is indicated in men with advanced hormone‑dependent prostate cancer, where androgen deprivation therapy is required. Degarelix’s profile and rapid onset of testosterone suppression make it an important option in clinical settings where immediate reduction of circulating testosterone is clinically beneficial and flare‑related complications are a concern.
Background and Date of Approval
Degarelix was developed as a long‑acting GnRH receptor antagonist for androgen deprivation therapy. It received regulatory approval from the United States Food and Drug Administration on 24 December 2008 for the treatment of advanced prostate cancer in adult male patients. The mechanism and clinical utility were supported by pivotal phase III trials demonstrating effective and sustained suppression of testosterone to castrate levels without testosterone flare, which underpinned its regulatory acceptance. Subsequent approvals by other agencies, including Japan’s regulatory authority by mid‑2012 and marketing authorisation opinions in Europe by 2023, have expanded its international use. These regulatory milestones reflect accumulated evidence of efficacy and safety in hormone‑dependent prostate carcinoma.
Uses
Degarelix is indicated for the treatment of adult male patients with advanced hormone‑dependent prostate cancer who require androgen deprivation therapy. In this setting, it is used to rapidly reduce circulating testosterone without the initial hormone surge seen with GnRH agonists. It may be employed as monotherapy or in combination with other approved anti‑androgen treatments, depending on clinical judgement and patient‑specific factors. Degarelix is generally not used in early localized prostate cancer outside its approved indication.
Administration
Degarelix is administered by subcutaneous injection. The typical regimen begins with a loading dose of 240 mg, usually given as two separate 120 mg injections, followed by monthly maintenance doses of 80 mg administered every 28 days. The initial and maintenance dosing schedule aims to rapidly achieve and maintain serum testosterone suppression to below castration levels. Treatment is continued until disease progression or unacceptable toxicity, with appropriate periodic clinical assessments guiding ongoing management.
Side Effects
Common side effects reported with degarelix include injection site reactions such as pain, redness, or swelling, and symptoms related to testosterone suppression including hot flashes, decreased libido, erectile dysfunction, nausea, diarrhea, weight gain, fatigue, and fluid retention. Mild elevations in liver enzymes and other metabolic changes may also occur. The severity and incidence of these effects vary among individuals and are generally manageable under medical supervision.
Warnings
Degarelix has serious adverse event considerations including hypersensitivity reactions, QT interval prolongation, and significant hormone‑related effects leading to complications such as severe hot flashes or metabolic changes. Hormone suppression can also impact bone density and cardiovascular risk profiles, requiring clinical evaluation and management. Degarelix is contraindicated in women, especially during pregnancy, due to its mechanism on hormone pathways, and effective contraception should be maintained for men of reproductive potential where appropriate. Treatment should be interrupted or discontinued in the event of life‑threatening toxicity.
Precautions
Before initiating degarelix, clinicians should assess baseline cardiovascular status, electrolytes, liver function, and QT interval due to potential risks. Caution is advised in patients with significant cardiac history or predisposition to arrhythmias. Degarelix does not typically undergo significant cytochrome P450 metabolism and classical small‑molecule drug interactions are uncommon, but concurrent medications that prolong the QT interval or alter hormonal status should be reviewed. Regular monitoring for changes in prostate‑specific antigen levels, testosterone levels, and clinical signs of toxicity or metabolic disturbances is recommended throughout treatment.
Expert Tips
When prescribing degarelix, it is important to confirm indication, counsel patients about the subcutaneous injection process, and discuss the expected timeline of testosterone suppression effects and potential hormonal side effects. Establish baseline ECG, liver function, electrolyte profiles, and bone health as part of the pretreatment assessment. Monitor patients regularly for injection site reactions, metabolic changes, cardiovascular status, and serum testosterone to ensure castrate levels are maintained. Educate patients about symptom reporting for potential serious events such as severe hot flashes, cardiac symptoms, or significant weight changes. Coordination with multidisciplinary care teams enhances safety and therapeutic effectiveness.
