Eribulin
Overview
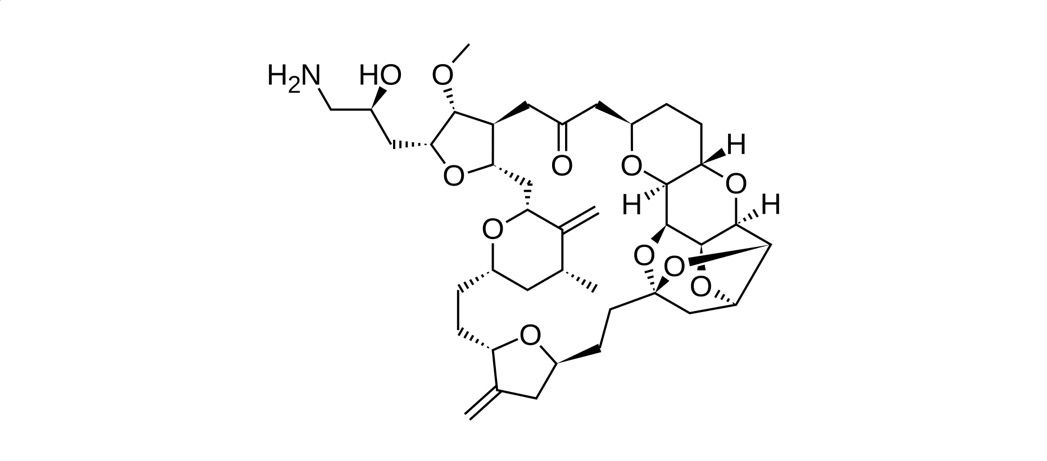
Eribulin is a cytotoxic antineoplastic agent that inhibits microtubule growth, leading to disruption of mitotic spindle formation and cell cycle arrest in rapidly dividing cancer cells. It is a synthetic analogue derived from a naturally occurring marine compound and is administered intravenously in oncology settings. Eribulin is clinically important for patients with advanced or metastatic cancers who have previously received standard chemotherapy, as it offers a treatment option when disease has progressed despite prior therapies. Its mechanism differs from taxanes and vinca alkaloids, allowing activity in tumors resistant to other microtubule-targeting agents. Because eribulin affects rapidly dividing cells, its use requires careful monitoring of blood counts and overall patient tolerance under specialist supervision.
Background and Date of Approval
Eribulin mesylate was developed following research into marine-derived compounds with antitumor activity. It received regulatory approval in the United States in 2010 for the treatment of metastatic breast cancer in patients previously treated with anthracycline- and taxane-based chemotherapy. Subsequent approvals were granted in multiple regions worldwide based on clinical trial data demonstrating improved overall survival compared with alternative treatments. In 2016, approval was expanded to include the treatment of unresectable or metastatic liposarcoma in patients who had received prior anthracycline-containing therapy, establishing its role in selected soft tissue sarcomas.
Uses
Eribulin is indicated for the treatment of adult patients with metastatic breast cancer who have previously received at least two chemotherapy regimens for metastatic disease, including an anthracycline and a taxane. It is also indicated for patients with unresectable or metastatic liposarcoma who have been treated with a prior anthracycline-containing regimen. Eribulin is typically used as monotherapy in these settings and is prescribed by oncology specialists as part of advanced cancer management.
Administration
Eribulin is administered by intravenous injection by a qualified healthcare professional. The standard adult dose is based on body surface area and is given on Days 1 and 8 of a 21-day treatment cycle. The injection is delivered over a short duration through a peripheral or central venous line. Treatment continues until disease progression or unacceptable toxicity occurs. Dose delays, reductions, or discontinuation may be required in response to hematologic toxicity, hepatic impairment, or other clinically significant adverse effects.
Side Effects
Common side effects associated with eribulin include fatigue, weakness, nausea, constipation, hair loss, peripheral neuropathy with numbness or tingling in the extremities, abdominal discomfort, and fever. Decreases in white blood cell counts, anemia, and electrolyte abnormalities are also frequently observed. The severity and combination of side effects vary between patients and are often manageable with supportive care, dose modification, and close monitoring.
Warnings
Serious adverse events with eribulin include severe neutropenia, febrile neutropenia, and life-threatening infections related to bone marrow suppression. Prolongation of the QT interval has been reported and may increase the risk of cardiac arrhythmias in susceptible patients. Severe peripheral neuropathy may occur with cumulative exposure and may require treatment interruption or discontinuation. Eribulin can cause embryo-fetal toxicity, and exposure during pregnancy should be avoided.
Precautions
Baseline evaluation before starting eribulin should include complete blood counts, electrolyte levels, and assessment of liver and kidney function. Blood counts should be monitored regularly during treatment, particularly prior to each dose. Caution is advised in patients with cardiac risk factors or electrolyte imbalances due to the potential for QT prolongation. Although eribulin has a low potential for classic drug–drug interactions, concomitant medications should be reviewed for overlapping toxicities. Effective contraception is required during treatment and for a period after therapy.
Expert Tips
Confirm adequate baseline hematologic recovery before each treatment cycle and delay dosing when neutropenia is present. Counsel patients on recognizing early signs of infection, neuropathy, and cardiac symptoms and advise prompt reporting. Coordinate supportive care measures, including growth factor support when appropriate, to maintain treatment intensity. Reinforce reproductive risk counseling and ensure coordination among oncology, pharmacy, and nursing teams to optimize safe administration.
