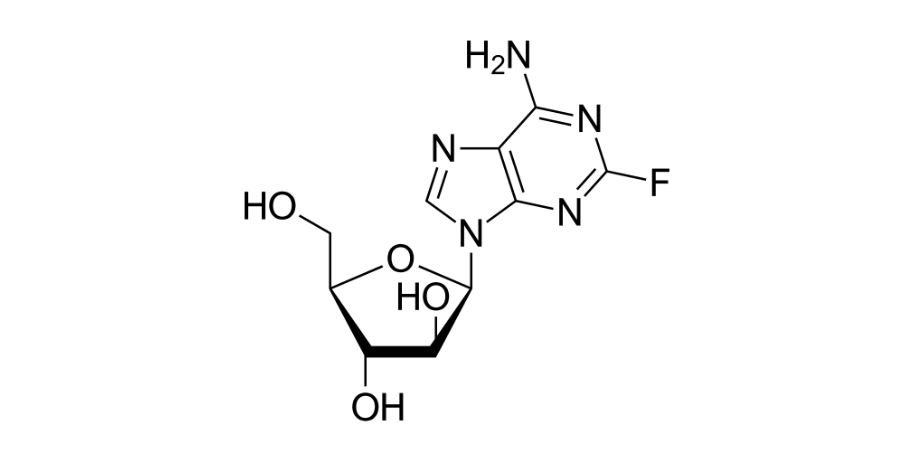
Fludarabine
Overview
Fludarabine is a synthetic purine analog antimetabolite chemotherapy agent that interferes with the synthesis and repair of DNA in malignant cells, leading to inhibition of tumor cell proliferation and induction of apoptosis. It is typically administered intravenously under clinical supervision and may also be available in oral form for specific indications. Fludarabine is rapidly dephosphorylated to an active metabolite that is then phosphorylated within cells to a triphosphate form, which competitively inhibits DNA polymerases and ribonucleotide reductase, disrupting DNA chain elongation and reducing the pool of nucleotides necessary for DNA synthesis. This mechanism targets rapidly dividing hematologic cancer cells, particularly malignant lymphocytes in chronic lymphocytic leukemia, and contributes to its utility in combination regimens. Fludarabine’s pharmacologic profile has also made it a key agent in certain transplant conditioning and lymphodepletion protocols due to its ability to suppress immune cells effectively.
Background and Date of Approval
Fludarabine was first approved by the United States Food and Drug Administration in 1991 as fludarabine phosphate for the treatment of adult patients with B‑cell chronic lymphocytic leukemia (CLL) who have not responded to or whose disease has progressed during treatment with at least one standard alkylating‑agent containing regimen. Subsequent regulatory updates, including revised labeling in 2024 under an FDA Project Renewal initiative, have expanded and clarified its use in combination regimens for CLL and updated recommended dosages with agents such as cyclophosphamide and rituximab. Fludarabine has been used for decades in hematologic oncology and is also incorporated into conditioning regimens for hematopoietic stem cell transplantation and lymphodepletion prior to certain cellular therapies.
Uses
Fludarabine is indicated for the treatment of adult patients with B‑cell chronic lymphocytic leukemia, especially in those whose disease has not responded to or progressed during treatment that included an alkylating agent. It is used as a component of combination chemotherapy regimens, including those paired with cyclophosphamide and rituximab in CLL. Off‑label uses in clinical practice include incorporation into conditioning regimens prior to hematopoietic stem cell transplantation and lymphodepletion before adoptive cellular therapies, taking advantage of its lymphocyte‑suppressive effects.
Administration
Fludarabine is administered by intravenous infusion under clinical supervision. A commonly used adult dosing regimen for chronic lymphocytic leukemia is 25 milligrams per square meter of body surface area given intravenously over approximately 30 minutes once daily for five consecutive days, repeated every 28 days, with continuation based on clinical response and tolerability. Dose adjustments or treatment interruptions may be required for hematologic toxicity or organ dysfunction. In conditioning or lymphodepletion regimens, dosing and schedules are tailored to specific protocols that may differ from standard CLL regimens. Baseline and ongoing assessments of blood counts and organ function guide dose modifications.
Side Effects
Common side effects associated with fludarabine therapy include myelosuppression leading to low blood cell counts such as anemia, neutropenia, and thrombocytopenia, which increase the risk of infection and bleeding. Other frequently observed effects include nausea, vomiting, diarrhea, fatigue, fever, chills, rash, and loss of appetite. The incidence and severity of these effects vary among individuals and are influenced by concomitant therapies and overall disease burden.
Warnings
Serious adverse events with fludarabine include profound and prolonged bone marrow suppression, severe infections, and hematologic toxicity. Rare but life‑threatening effects include central nervous system toxicity at high doses, autoimmune hemolytic anemia, pulmonary toxicity, and severe neurologic effects such as confusion or coma. Because of its potent immunosuppressive properties, fludarabine carries significant risk of opportunistic infections and requires careful clinical monitoring and supportive care. It is contraindicated in patients with known hypersensitivity to fludarabine or severe renal impairment, and use in pregnancy is associated with potential fetal harm.
Precautions
Before initiating fludarabine, baseline complete blood counts, liver and kidney function tests, and assessment of infection risk are essential. Special precautions are necessary in patients with pre‑existing immunosuppression, active infection, or significant organ dysfunction. Concomitant use of other myelosuppressive agents may exacerbate hematologic toxicity and should be carefully considered. Pneumocystis jirovecii pneumonia prophylaxis, antiviral prophylaxis, and other supportive measures may be indicated based on clinical context. Live vaccines should be avoided during significant immunosuppression. Regular clinical and laboratory follow‑up is required to detect and manage toxicities early in the course of treatment.
Expert Tips
Patient selection for fludarabine therapy involves confirming an appropriate hematologic indication and assessing baseline marrow reserve, renal function, and infection risk. Close monitoring of blood counts, signs of infection, and organ function throughout treatment helps guide dose adjustments and supportive interventions. Counseling patients about potential side effects, signs of infection, and the importance of adherence to monitoring schedules enhances safety. Coordination with multidisciplinary teams, including hematologists, pharmacists, and transplant specialists, improves outcomes in complex treatment plans. Supportive care strategies such as growth factor support and antimicrobial prophylaxis tailored to individual risk profiles are important aspects of clinical management.
