Fulvestrant
Overview
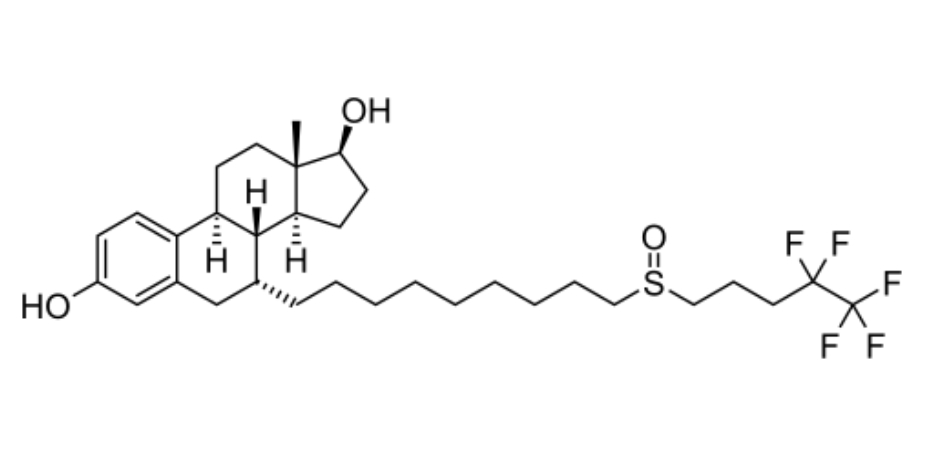
Fulvestrant is a synthetic estrogen receptor antagonist classified as a selective estrogen receptor degrader. It binds competitively to estrogen receptors on hormone receptor‑positive breast cancer cells and accelerates receptor degradation, thereby blocking estrogen signaling and inhibiting tumor cell proliferation. Unlike selective estrogen receptor modulators such as tamoxifen, fulvestrant has no partial agonist activity and is considered a pure antiestrogen. It is administered by deep intramuscular injection, typically into the gluteal muscles. Clinically, fulvestrant is important in the treatment of advanced hormone receptor‑positive, HER2‑negative breast cancer, particularly after progression on prior endocrine therapy. The mechanism of action includes high‑affinity binding to the estrogen receptor, downregulation of receptor expression, and disruption of estrogen‑driven gene transcription, contributing to reduced cancer cell growth and delayed disease progression. Fulvestrant’s targeted antiestrogen effects make it a cornerstone endocrine therapy in appropriate patient populations.
Background and Date of Approval
Fulvestrant was first approved by the United States Food and Drug Administration in 2002 for the treatment of hormone receptor‑positive metastatic breast cancer in postmenopausal women with disease progression following antiestrogen therapy. Subsequent regulatory approvals expanded its use to include combination therapy with CDK4/6 inhibitors such as ribociclib, palbociclib, and abemaciclib for hormone receptor‑positive, HER2‑negative advanced or metastatic breast cancer, either as initial endocrine-based therapy or after prior endocrine therapy progression. Approval decisions were based on clinical trials demonstrating improved disease control and acceptable safety profiles. These approvals established fulvestrant as a key therapy in modern endocrine management of advanced breast cancer.
Uses
Fulvestrant is indicated for the treatment of hormone receptor‑positive, HER2‑negative advanced or metastatic breast cancer in postmenopausal women. It is used as monotherapy for patients whose disease has progressed after prior endocrine therapy and in combination with CDK4/6 inhibitors as initial endocrine-based therapy or following disease progression on endocrine therapy. These indications reflect its role in managing estrogen-dependent breast cancer where suppression of estrogen signaling is therapeutically beneficial.
Administration
Fulvestrant is administered by deep intramuscular injection into the buttocks. The recommended dose is 500 mg given as two 5 mL injections, one in each buttock, administered slowly over 1 to 2 minutes on Days 1, 15, and 29, and then once monthly thereafter. When used in combination with CDK4/6 inhibitors, the same dosing schedule for fulvestrant is followed alongside the companion agent’s dosing regimen. In patients with moderate hepatic impairment, a reduced dose may be considered. Fulvestrant injections are given by healthcare professionals due to the administration technique and volume.
Side Effects
Common side effects observed with fulvestrant include injection site reactions, nausea, fatigue, headache, musculoskeletal pain, back pain, hot flashes, anorexia, constipation, diarrhea, cough, and dyspnea. Elevations in liver enzymes occur in some patients and are typically asymptomatic. These adverse effects reflect the drug’s antiestrogen activity and are typically manageable with supportive care and clinical monitoring.
Warnings
Serious adverse events associated with fulvestrant include hypersensitivity reactions and rare instances of significant hepatotoxicity with elevated liver enzymes. Use in patients with bleeding disorders, thrombocytopenia, or concurrent anticoagulant therapy warrants caution due to bleeding risk. Fulvestrant is contraindicated during pregnancy and in women who are breastfeeding due to potential harm to the fetus or infant. Treatment should be interrupted or discontinued if severe toxicities occur.
Precautions
Baseline assessments before initiating fulvestrant include liver function tests, evaluation of bleeding risk, and a review of concomitant medications. Patients with hepatic impairment may require dose adjustments. Live vaccines should be avoided during therapy due to potential immune effects. Drug interactions with fulvestrant are limited, but caution is advised when combining with therapies that may increase bleeding risk or impact liver function. Patients should be counselled on reporting symptoms of liver dysfunction or hypersensitivity.
Expert Tips
Patient selection should confirm hormone receptor‑positive, HER2‑negative disease and consider prior endocrine therapy history. Healthcare professionals should educate patients on the importance of adherence to the injection schedule and monitor for adverse effects, particularly liver enzyme elevations and injection site issues. Coordination with combination therapy partners such as CDK4/6 inhibitors requires awareness of overlapping toxicities and consistent follow‑up. Pharmacists should ensure proper storage and handling of injectable preparations and counsel patients on side effect expectations and management strategies.
