Ibrutinib
Overview
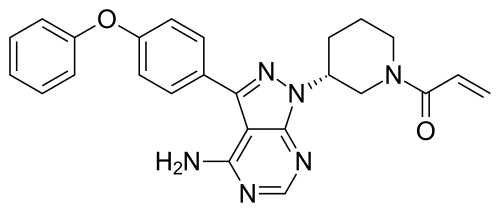
Ibrutinib is an oral small-molecule medicine classified as a Bruton's tyrosine kinase (BTK) inhibitor. It is widely used in oncology for the treatment of various B-cell malignancies, including chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and Waldenström’s macroglobulinemia (WM). Ibrutinib works by blocking BTK signaling, which is essential for the survival and proliferation of malignant B-cells. It is administered orally once daily, offering a convenient alternative to infusion-based therapies. Ibrutinib has transformed the treatment landscape for patients with difficult-to-treat blood cancers, with clinical trials demonstrating significant improvements in progression-free survival and overall response rates.
Background and Date of Approval
Ibrutinib was first approved by the U.S. Food and Drug Administration (FDA) in 2013 for mantle cell lymphoma, followed by subsequent approvals for CLL, WM, and other indications. It later gained European Medicines Agency (EMA) approval and is approved by the Drug Controller General of India (DCGI). The mechanism of action involves irreversible inhibition of Bruton's tyrosine kinase, a critical enzyme in the B-cell receptor signaling pathway. By blocking BTK, Ibrutinib disrupts malignant B-cell growth, migration, and survival. Major clinical trials such as RESONATE and HELIOS established its efficacy, showing durable remissions and improved survival outcomes compared with traditional chemotherapy-based regimens. Today, Ibrutinib is considered a backbone therapy in hematology and is often used as monotherapy or in combination with agents such as rituximab, obinutuzumab, or venetoclax.
Uses
Ibrutinib is indicated for adults with chronic lymphocytic leukemia, including those with 17p deletion, mantle cell lymphoma in patients who have received at least one prior therapy, Waldenström’s macroglobulinemia, marginal zone lymphoma in patients requiring systemic therapy after at least one anti-CD20-based regimen, and chronic graft-versus-host disease after failure of systemic therapy. Off-label, it has also been investigated in autoimmune diseases and other hematological malignancies, though such uses require further evidence.
Administration
Ibrutinib is taken orally once daily, usually at a dose of 420 mg for CLL and WM, and 560 mg for mantle cell lymphoma. Tablets or capsules should be swallowed whole with water at the same time each day. Food does not significantly affect absorption, but consistent administration is recommended. Dose adjustments may be required in patients with hepatic impairment or when used with interacting drugs. Treatment is typically continued until disease progression or unacceptable toxicity, making regular monitoring essential.
Side Effects
Patients may experience diarrhea, fatigue, musculoskeletal pain, bruising, rash, and nausea. Mild infections such as upper respiratory tract infections are common during treatment. These side effects are usually manageable and may improve over time, but persistent or worsening symptoms should be reported to a healthcare professional.
Warnings
Ibrutinib is associated with an increased risk of bleeding, atrial fibrillation, hypertension, and severe infections. Cases of tumor lysis syndrome have been reported in high-risk patients. It should be used with caution in individuals with cardiovascular disease or those requiring anticoagulants. There is a risk of secondary primary malignancies including skin cancers. Dose interruption or discontinuation may be required in cases of severe adverse reactions.
Precautions
Ibrutinib should be avoided in pregnancy and breastfeeding due to potential fetal harm. Caution is required in patients with liver disease as metabolism occurs primarily via CYP3A4. Strong CYP3A inhibitors such as ketoconazole and clarithromycin can significantly increase plasma concentrations of Ibrutinib, while inducers like rifampin may reduce efficacy. Grapefruit and Seville oranges should also be avoided due to CYP3A interaction. Regular monitoring of blood counts, liver function, and cardiovascular status is recommended during therapy.
Expert Tips
When initiating Ibrutinib, assess bleeding risk and cardiac history carefully. Educate patients on recognizing signs of atrial fibrillation, infection, and unusual bruising. Advise consistent adherence to daily dosing and caution against self-adjusting doses. Pharmacists should counsel patients on avoiding drug interactions and monitor for overlapping toxicities if used in combination regimens. Supportive care, including prophylactic antimicrobials in high-risk individuals, may be necessary.
