Idelalisib
Overview
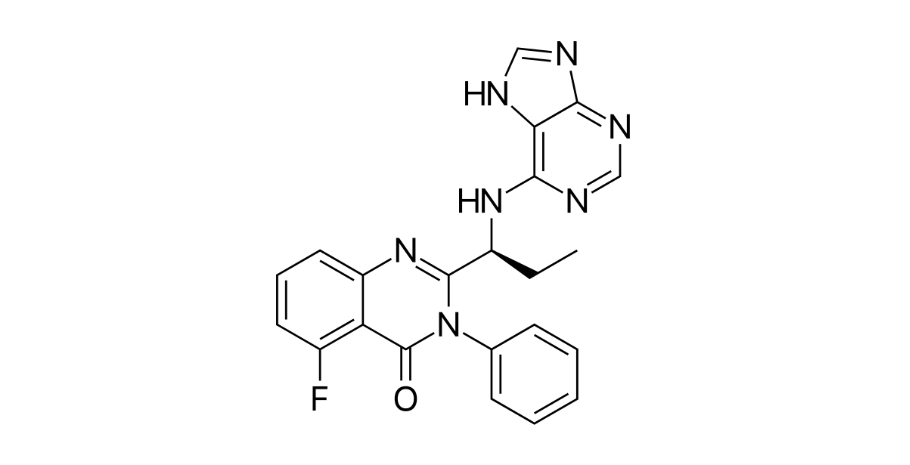
Idelalisib is an orally bioavailable small-molecule inhibitor of the phosphoinositide 3-kinase delta (PI3Kδ) enzyme, which plays a key role in intracellular signaling that regulates proliferation, survival, migration, and homing of malignant B cells. By selectively inhibiting PI3Kδ, idelalisib disrupts the B-cell receptor signaling cascade, reducing proliferation and inducing apoptosis in malignant B cells. As the first approved PI3Kδ inhibitor, idelalisib provides a targeted option for patients with certain relapsed or refractory B-cell malignancies who have limited responses to prior therapies. Its oral route allows outpatient administration under careful monitoring. The mechanism of idelalisib represents a shift from conventional cytotoxic chemotherapy to pathway-focused targeted therapy in hematologic oncology, providing efficacy while requiring vigilance for specific toxicities.
Background and Date of Approval
Idelalisib, developed by Gilead Sciences and marketed as Zydelig, received initial approval in 2014. The United States Food and Drug Administration approved it on July 23, 2014, for relapsed chronic lymphocytic leukemia in combination with rituximab, and for relapsed follicular lymphoma and small lymphocytic lymphoma as monotherapy under accelerated approval. The European Medicines Agency authorised idelalisib for similar indications in the same year. Continued approval for accelerated indications requires confirmatory evidence from clinical trials. Pivotal clinical studies demonstrated clinical benefit in relapsed B-cell malignancies, supporting its regulatory approvals.
Uses
Idelalisib is indicated for adult patients with relapsed chronic lymphocytic leukemia in combination with rituximab when rituximab alone is considered appropriate due to comorbidities. It is also approved as monotherapy for relapsed follicular B-cell non-Hodgkin lymphoma and relapsed small lymphocytic lymphoma in patients who have received at least two prior systemic therapies. Idelalisib is typically used in patients whose disease has progressed after standard treatments, offering a targeted approach in later-line therapy.
Administration
Idelalisib is administered orally in the form of film-coated tablets, with or without food. The recommended dose is 150 milligrams twice daily, approximately 12 hours apart. Treatment continues until disease progression or unacceptable toxicity. Dose modifications or temporary interruptions may be required for adverse effects, and in some cases a reduced dose of 100 milligrams twice daily may be considered. Baseline and ongoing clinical and laboratory monitoring is essential to guide safe dosing and manage toxicities.
Side Effects
Common adverse effects include diarrhea, nausea, fatigue, cough, fever, rash, abdominal discomfort, neutropenia, elevated liver enzymes, and symptoms related to infections. The severity and frequency of these effects vary among patients. Most are manageable under appropriate medical supervision with supportive care and dose adjustments when required.
Warnings
Serious toxicities associated with idelalisib include severe hepatotoxicity, severe diarrhea or colitis, pneumonitis, and intestinal perforation. Early identification of liver injury and gastrointestinal toxicity is essential, and interruption or discontinuation of therapy may be required. Increased risk of serious infections has been reported. Idelalisib is contraindicated in situations where first-line treatment is indicated and carries risks that require close clinical monitoring.
Precautions
Baseline assessments should include complete blood counts, liver and renal function tests, and infection risk evaluation. Special caution is needed in patients with pre-existing liver disease, gastrointestinal conditions, or immunosuppression. Live vaccines should generally be avoided. Concomitant use with other hepatotoxic drugs may increase liver injury risk. Careful review of all medications is recommended before initiating therapy.
Expert Tips
Patient selection requires confirmation of relapsed disease after prior therapy and assessment of overall fitness and organ function. Baseline and ongoing monitoring of liver enzymes, blood counts, and signs of infection or gastrointestinal toxicity is essential. Patients should report diarrhea, abdominal pain, respiratory symptoms, or fever immediately. Coordinating supportive measures such as antimicrobial prophylaxis and nutritional support may improve tolerability. Adherence to dosing schedules and proper management of toxicities enhances safety. Idelalisib should be prescribed with a clear plan for ongoing assessment and monitoring.
