Imatinib
Overview
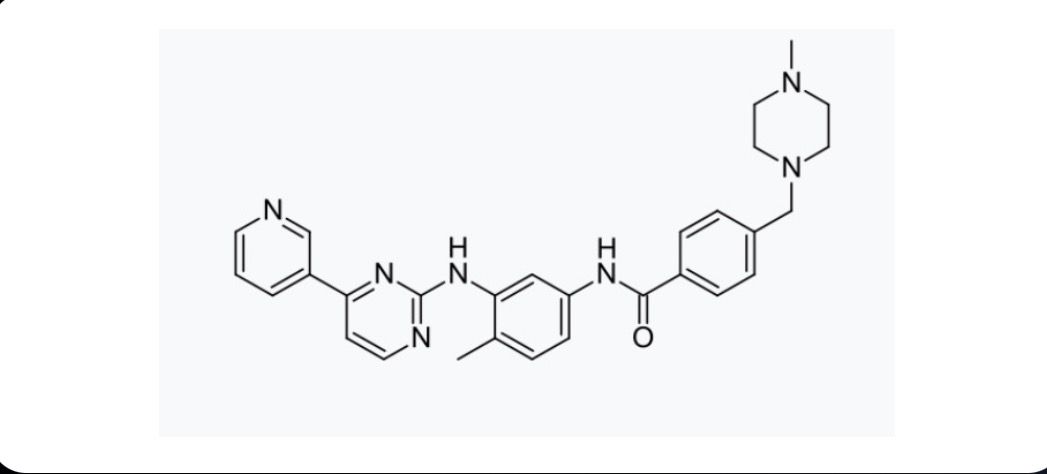
Imatinib is an oral targeted therapy classified as a tyrosine kinase inhibitor. It works by blocking abnormal proteins that drive the growth of cancer cells, particularly the BCR-ABL fusion protein found in chronic myeloid leukemia. By inhibiting this enzyme, imatinib slows or stops the growth of cancer cells while sparing normal cells to a greater extent than traditional chemotherapy. Imatinib has revolutionized the treatment of several cancers and is widely regarded as one of the most significant advances in oncology over the last two decades.
Background and Date of Approval
Imatinib was developed as one of the first rationally designed targeted cancer therapies. It received approval from the U.S. Food and Drug Administration in 2001 for the treatment of chronic myeloid leukemia. Its approval marked a turning point in precision oncology, demonstrating the potential of drugs that directly target the genetic drivers of cancer. Since then, imatinib’s use has expanded to multiple cancers, and it remains a cornerstone of therapy for hematological malignancies. Clinical trials and real-world studies consistently show its effectiveness in achieving long-term remission and improving overall survival.
Uses
Imatinib is primarily indicated for chronic myeloid leukemia in adults and children. It is also approved for the treatment of Philadelphia chromosome–positive acute lymphoblastic leukemia. Beyond hematologic cancers, imatinib is widely used for gastrointestinal stromal tumors, dermatofibrosarcoma protuberans, myelodysplastic/myeloproliferative diseases associated with PDGFR gene rearrangements, and systemic mastocytosis in selected patients. Its broad spectrum of activity against different tyrosine kinases allows it to be effective across a range of rare cancers.
Administration
Imatinib is administered orally in tablet form, typically once daily. The dosage varies depending on the type and stage of cancer being treated. For chronic myeloid leukemia, the standard starting dose ranges from 400 mg to 600 mg per day, while higher doses may be required for advanced disease. It should be taken with food and a full glass of water to reduce gastrointestinal irritation. Treatment is generally long-term, and adherence to daily dosing is essential for optimal outcomes. Dose adjustments may be required based on tolerance, response, and organ function.
Side Effects
The most frequent side effects of imatinib include nausea, vomiting, diarrhea, muscle cramps, fatigue, skin rash, and swelling around the eyes or ankles. These side effects are usually mild to moderate and can often be managed with supportive care or dose adjustments. Gastrointestinal discomfort is common, which is why taking the medicine with food is recommended.
Warnings
Serious risks associated with imatinib include severe fluid retention, heart failure, liver toxicity, and cytopenias such as anemia, neutropenia, and thrombocytopenia. Rare but serious events include gastrointestinal bleeding, tumor lysis syndrome, and severe skin reactions. Patients with preexisting cardiac or hepatic conditions require close monitoring. Imatinib should not be used during pregnancy due to risk of harm to the developing fetus.
Precautions
Imatinib is metabolized by the CYP3A4 enzyme, and caution is needed when taken with strong inhibitors or inducers of this pathway. Grapefruit and certain medications may increase drug levels, leading to toxicity. Patients with liver or kidney impairment may require dose adjustments. Regular monitoring of blood counts, liver function tests, and fluid status is recommended during therapy. Male and female patients of childbearing potential should use effective contraception during treatment.
Expert Tips
Imatinib is most effective when patients adhere to daily dosing schedules. Prescribers should monitor for hematologic response in leukemia and radiologic response in solid tumors. Pharmacists should counsel patients about taking the drug with meals to minimize gastrointestinal side effects and stress the importance of not skipping doses. Close attention should be given to drug–drug interactions, particularly with antifungals, antibiotics, and anti-seizure medications.
