Insulin Degludec
Overview
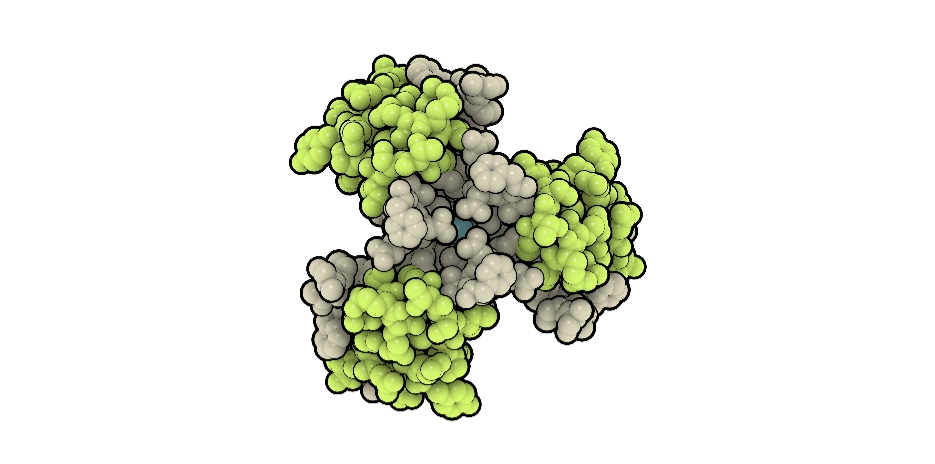
Insulin Degludec is an ultra long-acting recombinant basal insulin analogue designed to provide a consistent and prolonged insulin effect with minimal peak variation when administered subcutaneously. Unlike intermediate or some long-acting insulins, degludec forms multi-hexamers in subcutaneous tissue after injection, creating a steady depot from which insulin monomers are slowly released into the circulation. This mechanism provides a relatively flat, extended duration of action that can last up to approximately 42 hours, offering flexibility in daily dosing and helping maintain stable baseline glucose levels in patients with diabetes mellitus. Insulin Degludec is primarily used to support basal insulin needs in both type 1 and type 2 diabetes as part of an overall glycemic management plan that may also include prandial insulin or other therapies. Its long action profile and reduced variability help to decrease the frequency of nocturnal hypoglycemia and support simplified basal insulin regimens.
Background and Date of Approval
Insulin Degludec was developed by modifying the structure of human insulin to extend its duration of action and reduce peak concentrations, resulting in an ultra long-acting basal profile. It received regulatory approval from the United States Food and Drug Administration on 25 September 2015 for use in patients with diabetes mellitus aged one year and older. The European Medicines Agency approved Insulin Degludec earlier in 2013 for similar indications. These approvals were based on clinical trials demonstrating effective and stable glycemic control in both type 1 and type 2 diabetes with a lower incidence of nocturnal hypoglycemia compared with other basal insulins.
Uses
Insulin Degludec is indicated to improve glycemic control in adults and pediatric patients aged one year and older with type 1 diabetes mellitus and type 2 diabetes mellitus who require basal insulin therapy. It is used as part of comprehensive diabetes management to address baseline insulin deficiency and maintain fasting and between-meal glucose levels. Insulin Degludec is not indicated for the treatment of diabetic ketoacidosis. Dosing is individualized based on the patient’s metabolic needs, prior insulin use, and glycemic targets.
Administration
Insulin Degludec is administered by subcutaneous injection into the thigh, upper arm, or abdomen once daily at any time of day, preferably at the same time each day. The solution should be visually inspected and used only if clear and colorless. Injection sites should be rotated regularly to reduce the risk of lipodystrophy. Initial dosing in insulin-naive patients is individualized, with subsequent dose adjustments guided by blood glucose monitoring. In adults with type 2 diabetes, a commonly used starting dose is around 10 units once daily, with titration based on fasting glucose levels.
Side Effects
Common side effects associated with Insulin Degludec include hypoglycemia, which may present as sweating, tremors, dizziness, headache, hunger, or confusion. Injection site reactions such as redness, swelling, itching, or pain may occur. Weight gain can be observed as glycemic control improves. Other possible reactions include rash, pruritus, or peripheral edema.
Warnings
Serious adverse events include severe hypoglycemia, which can result in seizures, loss of consciousness, or death if untreated. Hypokalemia may occur due to insulin-mediated potassium shifts, potentially leading to cardiac rhythm disturbances. Fluid retention and worsening of heart failure have been reported when used with thiazolidinediones. Severe allergic or hypersensitivity reactions, including anaphylaxis, are rare but require immediate discontinuation. Insulin Degludec should not be used during episodes of hypoglycemia or in patients with known hypersensitivity to the drug or its components.
Precautions
Renal or hepatic impairment may alter insulin requirements and necessitate careful dose adjustment. Changes in diet, physical activity, body weight, or concurrent illness can affect glycemic control. Certain medications such as beta-blockers, corticosteroids, diuretics, and other antidiabetic drugs may influence insulin action or mask symptoms of hypoglycemia. Regular monitoring of blood glucose is essential to ensure safe and effective therapy.
Expert Tips
Insulin Degludec should be individualised based on patient-specific glycemic patterns and lifestyle considerations. Patients should be educated on correct injection technique, site rotation, and recognition of hypoglycemia symptoms. Dose adjustments should be made gradually, allowing sufficient time to reach steady-state insulin levels. Patients should be advised to carry fast-acting carbohydrates for prompt management of hypoglycemia. Multidisciplinary diabetes care can enhance adherence and long-term outcomes.
