Lenalidomide
Overview
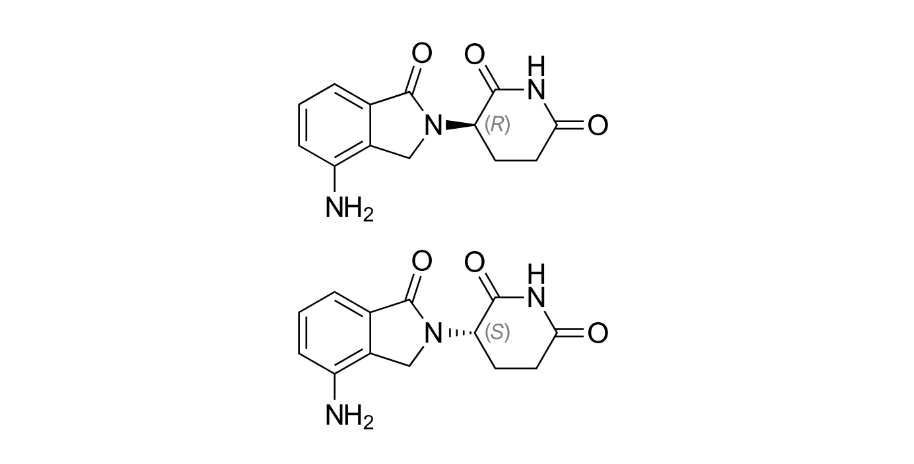
Lenalidomide is a synthetic analog of thalidomide with immunomodulatory, anti‑angiogenic, and antineoplastic properties that enhance anticancer immune responses and inhibit tumor cell proliferation. It modulates cytokine production, alters T‑cell and natural killer cell activation, and targets a cellular protein complex involving cereblon, leading to the degradation of specific transcription factors that support malignant cell survival. These combined effects reduce malignant cell growth and promote apoptosis in targeted hematologic tissues. Lenalidomide is administered orally and is a key component of treatment regimens for several blood cancers, often in combination with corticosteroids or other agents. Its multi‑faceted mechanism distinguishes it from traditional cytotoxic chemotherapy by harnessing both immunologic and direct tumor‑suppressing actions, making it vital in managing disease progression and improving clinical outcomes in a variety of hematologic malignancies.
Background and Date of Approval
Lenalidomide was first approved by the United States Food and Drug Administration on December 27, 2005 for the treatment of certain subtypes of myelodysplastic syndromes, including those with deletion of chromosome 5q. It received its next major approval on June 29, 2006 for use in combination with dexamethasone in adult patients with multiple myeloma who had received at least one prior therapy. Over the following years, regulatory updates expanded its indications, including approval for mantle cell lymphoma in 2013 and extension of its multiple myeloma indication to newly diagnosed patients who are not candidates for autologous stem cell transplant in 2015. On February 22, 2017, lenalidomide was approved as maintenance therapy for multiple myeloma following autologous stem cell transplant, reflecting its evolving role in long‑term disease management. These approvals were supported by pivotal randomized clinical trials demonstrating improved progression‑free survival and response rates compared with control regimens.
Uses
Lenalidomide is indicated for the treatment of adult patients with multiple myeloma in various settings, including in combination with dexamethasone for relapsed or refractory disease and as part of first‑line treatment regimens for newly diagnosed patients not eligible for transplant. It is also indicated in patients with myelodysplastic syndromes associated with deletion 5q abnormalities, where it can improve hematologic parameters, and for the treatment of mantle cell lymphoma after at least two prior therapies. In some regions and clinical practice settings, lenalidomide in combination with rituximab or other agents is used for indolent lymphomas such as follicular or marginal zone lymphoma following prior treatment failure. Use is tailored by disease type, prior therapies, and patient characteristics.
Administration
Lenalidomide is administered orally in capsule form, with common dosing tailored to the specific indication. For multiple myeloma, a typical regimen involves 25 milligrams once daily on days 1 through 21 of repeated 28‑day cycles, in combination with dexamethasone or as part of other defined regimens. In myelodysplastic syndromes with deletion 5q, dosing may be lower and continuous per labeled recommendations. Dose adjustments and interruptions are often necessary for hematologic toxicity, renal impairment, or other adverse effects. Baseline and ongoing assessments of blood counts, renal function, and clinical status are essential to guide safe dosing and ensure therapeutic balance.
Side Effects
Common side effects of lenalidomide include neutropenia, thrombocytopenia, anemia, fatigue, diarrhea, constipation, nausea, rash, and muscle or bone pain. Hematologic toxicities such as low white blood cell or platelet counts are among the most frequently observed adverse effects and can increase the risk of infection or bleeding. The incidence and severity of these effects vary among patients and are influenced by concomitant therapies and underlying disease status.
Warnings
Serious adverse events associated with lenalidomide include profound bone marrow suppression resulting in severe neutropenia and thrombocytopenia, increasing the risk of serious infection and bleeding. Venous and arterial thromboembolic events such as deep vein thrombosis, pulmonary embolism, myocardial infarction, and stroke have been reported, particularly when used with corticosteroids or other agents. Lenalidomide carries a significant risk of embryo‑fetal toxicity and is contraindicated in pregnancy; strict contraception measures are mandated for males and females of reproductive potential. Increased incidence of second primary malignancies, hepatotoxicity, and severe cutaneous reactions including Stevens‑Johnson syndrome and toxic epidermal necrolysis have been reported. Careful monitoring and prompt management of these events are critical to minimize morbidity.
Precautions
Prior to initiating lenalidomide, baseline complete blood counts, liver and kidney function tests, and assessment of thrombotic risk are essential. Special precautions are necessary in patients with significant renal impairment, as dose adjustments are often required, and in older patients who may have increased susceptibility to toxicity. Concomitant use of anticoagulants or agents affecting hematologic parameters should be carefully managed to balance bleeding and thrombotic risks. Live vaccines should generally be avoided during significant immunosuppression. Regular clinical and laboratory follow‑up is essential to detect cytopenias, organ dysfunction, or emergent adverse events early and guide therapeutic adjustments.
Expert Tips
Patient selection for lenalidomide therapy involves confirming a regulatory‑approved indication and assessing baseline bone marrow reserve, renal function, and thrombotic risk. Monitoring of complete blood counts prior to each cycle helps detect evolving cytopenias, and early intervention with dose modification or supportive care improves tolerability. Patients should be counselled on signs of infection, bleeding, and thromboembolism and advised to report symptoms promptly. Effective contraception is crucial for patients of reproductive potential due to teratogenic risk, and adherence to risk mitigation programs enhances safety. Coordination with multidisciplinary oncology teams ensures comprehensive management of adverse effects, and educating patients on common side effects and the importance of adherence fosters better clinical outcomes.
