Lenvatinib
Overview
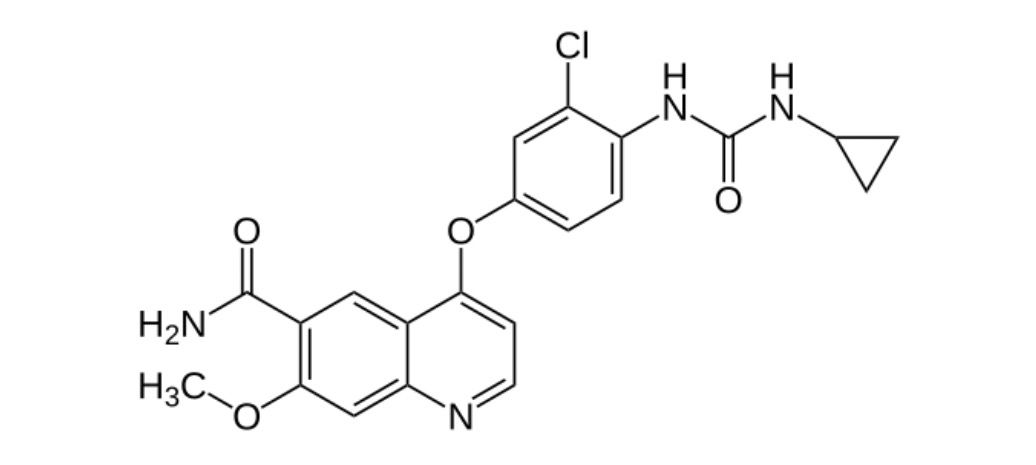
Lenvatinib is an oral multi-targeted receptor tyrosine kinase inhibitor that acts on VEGFR1–3, FGFR1–4, PDGFRα, RET, and KIT, proteins involved in tumor angiogenesis and growth. By blocking these pathways, lenvatinib helps slow tumor progression and improve outcomes in patients with advanced cancers. It is primarily used in differentiated thyroid cancer that is radioactive iodine-refractory, advanced renal cell carcinoma in combination with everolimus, and unresectable hepatocellular carcinoma. Lenvatinib’s targeted mechanism allows for effective therapy while maintaining manageable safety, making it a cornerstone in oncology treatment protocols.
Background and Date of Approval
Lenvatinib received its first FDA approval in 2015 for differentiated thyroid cancer (DTC) that is locally recurrent or metastatic and refractory to radioactive iodine therapy. Its efficacy in combination with everolimus for advanced renal cell carcinoma was approved in 2016, while first-line treatment for unresectable hepatocellular carcinoma gained FDA approval in August 2018. European Medicines Agency approvals followed similar timelines, confirming its role across these cancer indications. The clinical development of lenvatinib was guided by pivotal trials showing significant improvement in progression-free survival, tumor response rates, and patient outcomes across DTC, RCC, and HCC populations.
Uses
Lenvatinib is indicated for adult patients with progressive, radioactive iodine-refractory differentiated thyroid cancer, for those with advanced renal cell carcinoma in combination with everolimus following prior anti-angiogenic therapy, and as a first-line option for unresectable hepatocellular carcinoma. In differentiated thyroid cancer, lenvatinib provides a treatment option when radioactive iodine therapy is no longer effective. In renal cell carcinoma, its combination with everolimus enhances anti-tumor activity. In hepatocellular carcinoma, lenvatinib improves progression-free survival and overall response rates compared to sorafenib, demonstrating its broad utility in targeted cancer therapy.
Administration
For differentiated thyroid cancer, lenvatinib is administered orally at a recommended dose of 24 mg once daily, with dose adjustments based on tolerability. In combination therapy for renal cell carcinoma, the recommended dose is 18 mg once daily alongside everolimus 5 mg daily. For hepatocellular carcinoma, dosing is weight-based, with 12 mg once daily for patients weighing 60 kg or more, and 8 mg once daily for those under 60 kg. Therapy continues until disease progression or unacceptable toxicity. Close monitoring of blood pressure, liver and kidney function, and overall patient status is required, and dose interruptions or reductions are advised in case of severe adverse events.
Side Effects
Common side effects of lenvatinib include hypertension, fatigue, diarrhea, decreased appetite, nausea, stomatitis, headache, proteinuria, palmar-plantar erythrodysesthesia, arthralgia, myalgia, abdominal discomfort, and weight loss. These side effects vary across indications but are generally manageable with supportive care, treatment adjustments, and careful monitoring. Patients are advised to report persistent or severe symptoms to their healthcare provider promptly.
Warnings
Lenvatinib can cause serious hypertension that may require dose reduction, interruption, or discontinuation. Cardiac dysfunction, including reduced ejection fraction, has been reported, necessitating regular monitoring. Arterial thromboembolic events and hepatotoxicity are significant concerns and should prompt treatment modification or cessation. Renal impairment, proteinuria, diarrhea, gastrointestinal perforation, hemorrhagic events, and impaired wound healing are additional serious risks. Lenvatinib is contraindicated during pregnancy due to potential fetal harm.
Precautions
Patients should be evaluated for cardiovascular, hepatic, and renal function prior to starting therapy. Pre-existing hypertension must be controlled, and ongoing monitoring is essential. Electrolyte imbalances, thyroid function abnormalities, and history of gastrointestinal fistulas should be assessed. Concurrent use of medications that may exacerbate liver dysfunction or hypertension should be carefully managed. Patient education on early symptom recognition for serious adverse events is critical for safety.
Expert Tips
Before initiating therapy, clinicians should ensure baseline evaluations for blood pressure, liver and kidney function, and thyroid levels. Patients should be advised on signs of severe hypertension, proteinuria, gastrointestinal complications, and bleeding. Regular follow-up visits with laboratory monitoring are essential. Dose modifications should be promptly implemented in response to adverse events. Coordination with a multidisciplinary team including cardiologists, nephrologists, and endocrinologists can optimize treatment outcomes.
