Nilotinib
Overview
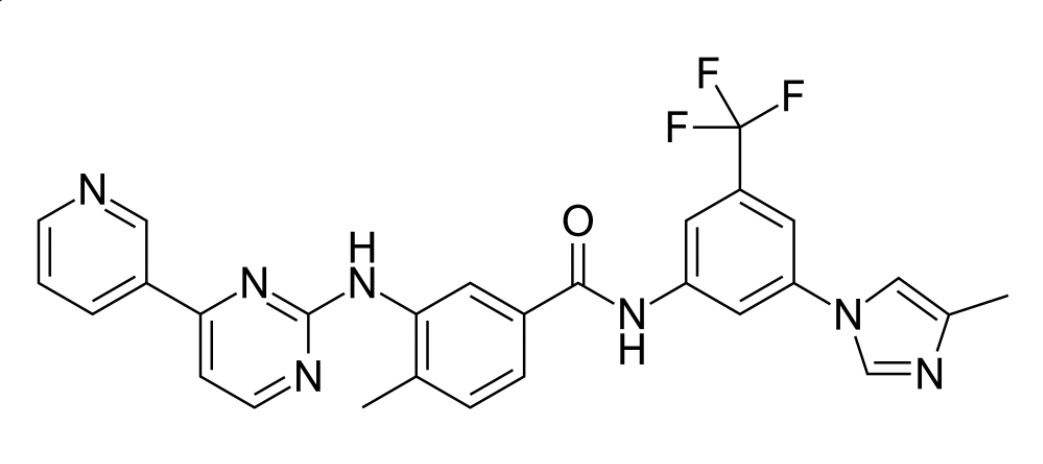
Nilotinib, marketed under the brand name Tasigna, is a tyrosine kinase inhibitor used in the treatment of Philadelphia chromosome-positive chronic myeloid leukemia (Ph+ CML). It works by inhibiting the BCR-ABL fusion protein, which is responsible for the uncontrolled proliferation of leukemic cells. By targeting this specific protein, nilotinib helps to control the progression of CML and improve patient outcomes.
Background and Date of Approval
Nilotinib was approved by the U.S. Food and Drug Administration (FDA) in 2007 for the treatment of Ph+ CML in chronic phase. Its approval was based on clinical trials demonstrating its efficacy in reducing the number of leukemic cells and improving hematologic and cytogenetic responses in patients. Since then, it has become a standard treatment option for patients with Ph+ CML who are resistant or intolerant to prior therapy, including imatinib.
Uses
Nilotinib is indicated for the treatment of adult and pediatric patients aged 1 year and older with newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase. It is also indicated for the treatment of adult patients with chronic phase and accelerated phase Ph+ CML who are resistant or intolerant to prior therapy that included imatinib. The effectiveness of nilotinib is based on hematologic and cytogenetic response rates.
Administration
Nilotinib should be taken orally twice daily at approximately 12-hour intervals. It must be taken on an empty stomach; no food should be consumed for at least 2 hours before and 1 hour after taking the dose. The recommended dose for newly diagnosed Ph+ CML is 300 mg twice daily. For resistant or intolerant Ph+ CML, the recommended dose is 400 mg twice daily. If a dose is missed, the patient should not take a make-up dose but should resume taking the next prescribed dose.
Side Effects
Common side effects of nilotinib include nausea, vomiting, diarrhea, constipation, rash, temporary hair loss, night sweats, and pain in bones, joints, or muscles. These side effects are generally manageable and may subside with continued therapy. Patients should be monitored regularly to assess and manage any adverse reactions.
Warnings
Serious adverse events associated with nilotinib include QT prolongation, which can lead to irregular heart rhythms, fainting, seizures, or sudden death. Other serious risks include low white blood cell counts, which increase the risk of infection, and low platelet counts, which can lead to bleeding. Patients should be monitored for these risks, and appropriate interventions should be implemented as needed.
Precautions
Before initiating therapy with nilotinib, a thorough assessment of the patient's medical history is essential, particularly concerning heart conditions and electrolyte imbalances. Concomitant use of strong CYP3A4 inhibitors or inducers should be approached with caution, as they can significantly affect nilotinib plasma concentrations. Regular monitoring of blood counts, liver function, and electrocardiograms is recommended during treatment.
Expert Tips
Prescribers should ensure that patients are adequately informed about the potential side effects of nilotinib and the importance of adhering to the prescribed dosing schedule. Pharmacists should counsel patients on proper administration techniques and the significance of regular follow-up appointments to monitor treatment efficacy and safety. Collaboration among healthcare providers is essential to optimize patient outcomes.
