Obinutuzumab
Overview
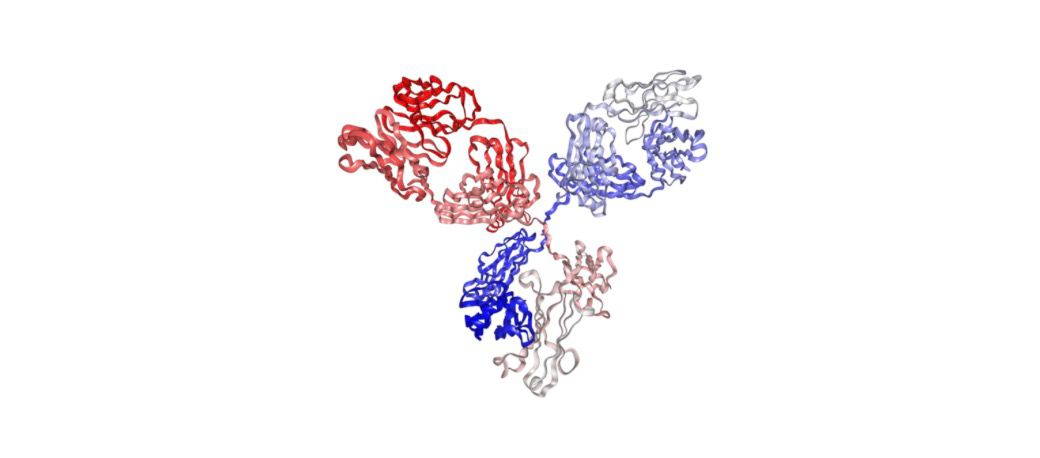
Obinutuzumab is an intravenous, glycoengineered type II anti-CD20 monoclonal antibody used to treat certain B-cell malignancies. It binds to CD20 on B lymphocytes and induces cell death through enhanced antibody-dependent cellular cytotoxicity, antibody-dependent cellular phagocytosis, and direct non-apoptotic cell death. Obinutuzumab is used in combination with chemotherapy for previously untreated chronic lymphocytic leukaemia (CLL) in patients unsuitable for full-dose fludarabine combinations and in combination with chemotherapy for follicular lymphoma in specific settings, and it is used as maintenance therapy in follicular lymphoma following induction. Infusion related reactions are common, particularly with the first infusion, and premedication and stepwise infusion rates are important to reduce risk. Other safety considerations include infection risk, hepatitis B reactivation, cytopenias, progressive multifocal leukoencephalopathy, and respiratory complications.
Background and Date of Approval
Obinutuzumab was first approved by the U.S. Food and Drug Administration on November 1, 2013 for use in combination with chlorambucil as first-line treatment for previously untreated CLL patients, marking the first FDA approval granted under Breakthrough Therapy designation. On February 26, 2016, the FDA expanded approval to include use in combination with bendamustine followed by obinutuzumab monotherapy for patients with follicular lymphoma who relapsed after or were refractory to a rituximab-containing regimen. Further, on November 16, 2017, regular approval was granted for first-line treatment of previously untreated stage II bulky, III, or IV follicular lymphoma when used with chemotherapy followed by obinutuzumab maintenance. These approvals were based on randomized clinical trials demonstrating improved progression-free survival and deeper response rates across patient populations.
Uses
Obinutuzumab is indicated for use in combination with chlorambucil for the treatment of previously untreated chronic lymphocytic leukaemia in patients for whom fludarabine-based therapy is considered unsuitable. It is indicated for treatment of follicular lymphoma in patients who have relapsed after prior therapy when given with chemotherapy and may be used as maintenance therapy following response to induction in certain clinical settings. Usage and approved lines of therapy vary by regulatory jurisdiction and should be checked against local prescribing information and patient eligibility criteria.
Administration
Obinutuzumab is administered by intravenous infusion under the supervision of a clinician experienced in cytotoxic therapy. For chronic lymphocytic leukaemia in combination with chlorambucil, the first infusion is commonly split with an initial test dose (for example a small portion on day 1) followed by completion of the first dose and subsequent infusions, with typical full doses of 1000 mg given on scheduled days during cycle one and on day 1 of subsequent cycles according to the approved regimen. For follicular lymphoma induction, the usual regimen includes 1000 mg infusions on days 1, 8, and 15 of cycle one followed by day 1 of subsequent cycles, and maintenance dosing often consists of 1000 mg every two months for up to two years in responders. Infusion rate should start slow and increase stepwise if tolerated, with interruption or slowing required for infusion related reactions. Premedication with a corticosteroid, antipyretic, and antihistamine is recommended before each infusion. Tumour lysis syndrome risk should be assessed and prophylaxis given when appropriate. Dose adjustments are based on severity of toxicity and clinical judgment.
Side Effects
Common adverse effects associated with obinutuzumab include infusion related reactions occurring most frequently with the first infusion, neutropenia, thrombocytopenia, anaemia, fever, chills, nausea, vomiting, cough, bronchospasm, fatigue, and musculoskeletal pain. Many adverse reactions are infusion-related and lessen with subsequent doses once tolerance is established. Cytopenias may require monitoring and temporary interruption of therapy.
Warnings
Serious risks include severe infusion related reactions that can be life threatening, serious infections including opportunistic infections, reactivation of hepatitis B virus with fulminant hepatitis and hepatic failure, progressive multifocal leukoencephalopathy, and severe cytopenias that can lead to bleeding or infection. Respiratory complications including interstitial lung disease and severe bronchospasm have been reported. Pregnancy may be adversely affected by monoclonal antibody therapy and effective contraception should be discussed. Vaccination response may be impaired and live vaccines should be avoided during and after treatment until immune recovery.
Precautions
Screen for active or prior hepatitis B infection prior to initiating therapy and monitor periodically during and after treatment. Provide prophylaxis and monitor for tumour lysis syndrome in patients at risk. Use caution in patients with a history of severe pulmonary disease, active infections, or significant cytopenias. Premedicate patients with corticosteroid, antihistamine, and antipyretic prior to infusion to reduce infusion related reactions. Avoid live vaccinations during and after treatment until immune function has recovered. Concomitant use with other immunosuppressive agents increases infection risk; review all concomitant medications and adjust management accordingly.
Expert Tips
Obtain hepatitis B screening and consider antiviral prophylaxis where indicated. Counsel patients about the high likelihood of infusion related reactions during the first infusion and the need for premedication and monitoring during and for 24 hours after infusion. Start infusions at a conservative rate for the first dose and increase gradually if tolerated; be prepared to slow or stop the infusion for reactions. Monitor complete blood counts at baseline and periodically during treatment and manage cytopenias per established guidance. Coordinate vaccination schedules to avoid live vaccines and discuss timing of inactivated vaccines with the treating team. Provide clear instructions on infection precautions and immediate reporting of fever or respiratory symptoms.
