Osimertinib
Overview
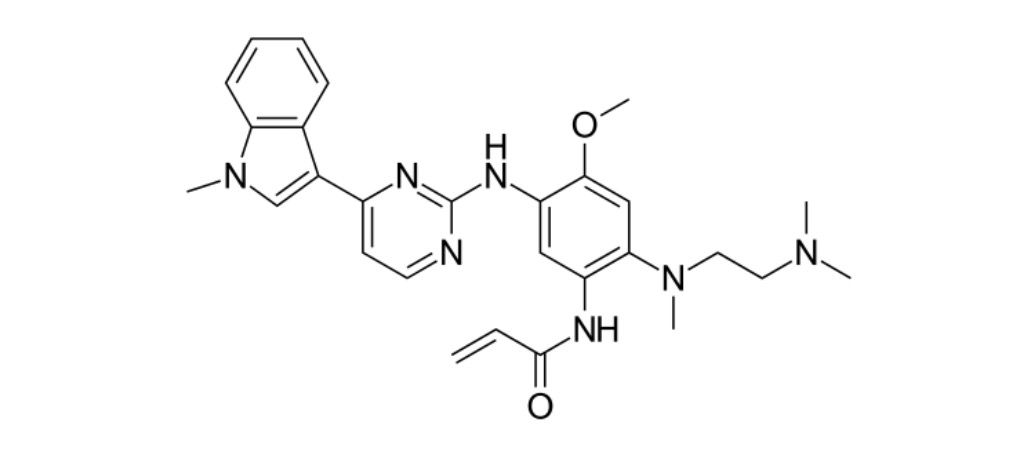
Osimertinib is an oral third-generation epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) that irreversibly targets both EGFR-sensitizing mutations (such as exon 19 deletions and exon 21 L858R) and the acquired resistance mutation T790M. By binding covalently to the C797 residue in the ATP-binding site of mutant EGFR, Osimertinib effectively blocks downstream signaling pathways (including PI3K/AKT/mTOR and RAS/RAF/MEK/ERK) that drive tumor cell survival and proliferation. Its high selectivity for mutant EGFR over wild-type homologs reduces off-target toxicity. Osimertinib crosses the blood-brain barrier, offering clinical benefit in central nervous system metastases. Its oral formulation, durable responses, and CNS activity have made it a foundational option in EGFR-mutant non-small cell lung cancer (NSCLC).
Background and Date of Approval
Osimertinib gained accelerated approval from the U.S. FDA in 2015 for treatment of metastatic EGFR T790M-positive NSCLC following progression on prior EGFR-TKI therapy. Full approval followed in 2017 after favorable benefit-risk assessment demonstrated robust response rates and tolerability. In 2018, Osimertinib became the first EGFR-TKI proven to improve survival in the first-line setting for EGFR-mutant metastatic NSCLC, becoming a new standard of care. In 2024, the FDA extended approval to include unresectable stage III EGFR-mutant NSCLC as maintenance therapy after chemoradiation. The FLAURA2 Phase III trial further supported Osimertinib combined with chemotherapy in first-line advanced disease, reinforcing its role across treatment stages.
Uses
Osimertinib is indicated for the adjuvant treatment of adult patients with resected early-stage NSCLC harboring EGFR exon 19 deletions or L858R mutations. It also serves as first-line therapy for metastatic NSCLC with these activating mutations. Osimertinib is indicated for metastatic T790M-positive NSCLC after progression on EGFR-TKI therapy. Recently, its use was approved in unresectable stage III NSCLC after chemoradiation, expanding benefit into earlier disease settings. In advanced disease, the combination of Osimertinib with platinum-based chemotherapy has demonstrated improved survival outcomes and may become a new standard in first-line treatment.
Administration
Osimertinib is administered orally at a standard dose of 80 mg once daily with or without food. Therapy continues until disease progression or unacceptable toxicity. Its pharmacokinetic profile includes a median time to maximum concentration of six hours, an elimination half-life around 48 hours, and primarily fecal excretion with some urinary elimination. Dosing remains consistent across settings, but regular monitoring and dose adjustments may be required based on adverse effects or drug interactions via CYP3A metabolism.
Side Effects
Common adverse effects observed in patients receiving Osimertinib include diarrhea, rash, dry skin, paronychia, stomatitis, nail toxicity, musculoskeletal pain, fatigue, and cough. These side effects typically develop early in therapy and are manageable with supportive care. Rash severity may correlate with efficacy in some studies. CNS adverse events are relatively uncommon but require vigilance given Osimertinib’s brain penetrance.
Warnings
Serious risks associated with Osimertinib include interstitial lung disease or pneumonitis, QT-interval prolongation, and cardiomyopathy, warranting baseline and periodic monitoring of lung and heart function. Fetal harm is likely; therefore, effective contraception is required during and after treatment. Patients should seek immediate medical attention for new or worsening respiratory symptoms or cardiac symptoms.
Precautions
Before initiating Osimertinib, evaluate baseline pulmonary and cardiac function, and correct electrolyte abnormalities. Concurrent use of strong CYP3A inhibitors or inducers should be approached cautiously due to potential changes in Osimertinib exposure. Watch for signs of pneumonitis, QTc prolongation, or heart dysfunction during therapy. Coordination with cardiology or pulmonology may be needed for high-risk patients.
Expert Tips
Confirm EGFR mutation status prior to starting Osimertinib, as its efficacy is mutation-specific. Patients should be counseled on dosing adherence, monitoring schedules, and signs of serious toxicity. Advise on skin care to manage dermatologic effects and recognize early signs of ILD or QT issues. Pharmacists should review concurrent medications for CYP3A interactions and advise accordingly. Coordinate multidisciplinary care for CNS metastases monitoring and supportive needs.
