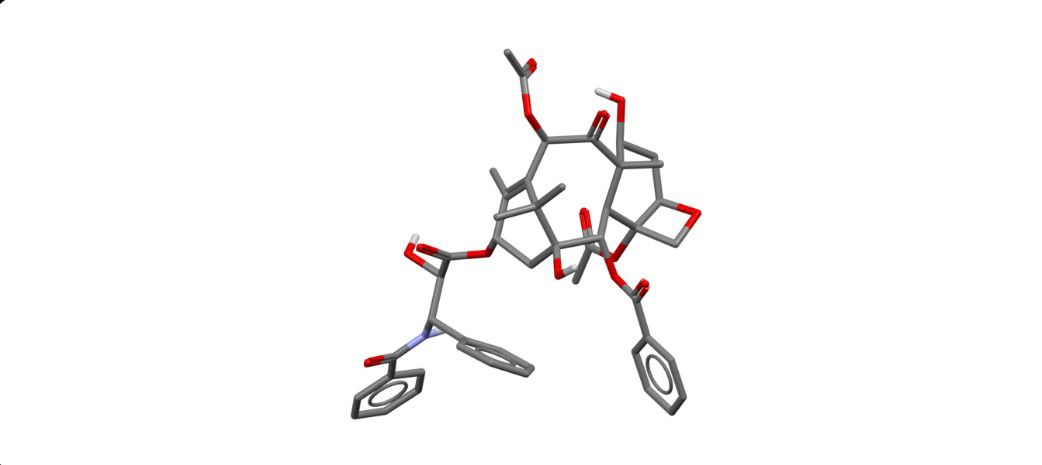
Paclitaxel
Overview
Paclitaxel is a cytotoxic chemotherapy agent that stabilizes microtubules and inhibits their depolymerization, effectively disrupting cell division and inducing apoptosis in rapidly dividing cancer cells. It is used in the treatment of breast cancer, ovarian cancer, non-small cell lung cancer, and other solid tumors. Paclitaxel can be administered intravenously and is often part of combination chemotherapy regimens to improve efficacy. Its role in oncology is well-established, offering significant survival benefits in multiple malignancies. Careful monitoring is required due to potential myelosuppression and other toxicities, but when administered appropriately, Paclitaxel is a cornerstone in standard cancer therapy protocols.
Background and Date of Approval
Paclitaxel was originally isolated from the bark of the Pacific yew tree and later developed into a clinically viable formulation. It received FDA approval in 1992 for the treatment of advanced ovarian cancer and subsequently for metastatic breast cancer and non-small cell lung cancer. Key clinical trials demonstrated improved progression-free and overall survival in treated populations. Paclitaxel’s mechanism of action as a microtubule stabilizer differentiated it from other chemotherapeutic agents, establishing it as an essential drug in oncology. Over the years, various formulations, including albumin-bound nanoparticle formulations, have been developed to improve solubility, reduce hypersensitivity reactions, and optimize delivery.
Uses
Paclitaxel is indicated for the treatment of ovarian cancer, metastatic breast cancer, non-small cell lung cancer, and Kaposi’s sarcoma. It is often used in combination with platinum-based chemotherapies or other cytotoxic agents to enhance treatment response. In breast cancer, it is commonly used in adjuvant and neoadjuvant settings to reduce recurrence risk. For ovarian cancer, Paclitaxel is combined with carboplatin as standard therapy. Its application is carefully tailored based on tumor type, stage, and patient performance status, ensuring optimal efficacy while minimizing adverse effects.
Administration
Paclitaxel is administered intravenously, with dosage regimens varying according to indication, patient weight, and combination therapy. Standard dosing ranges from 135 mg/m² to 175 mg/m², typically given every three weeks or on a weekly schedule depending on the protocol. Pre-medication with corticosteroids, antihistamines, and H2 blockers is required to reduce hypersensitivity reactions. Continuous monitoring of blood counts, liver function, and infusion site is essential. Dose adjustments may be necessary for patients with hepatic impairment or severe neutropenia.
Side Effects
Common adverse effects include neutropenia, anemia, thrombocytopenia, alopecia, nausea, vomiting, diarrhea, peripheral neuropathy, fatigue, and musculoskeletal pain. Mild hypersensitivity reactions, flushing, and transient fever may occur during infusion. Most side effects are manageable with supportive care, dose adjustments, or pre-medication. Patients should be advised to report persistent or severe symptoms promptly.
Warnings
Serious risks include severe myelosuppression, infections due to neutropenia, cardiac toxicity, hypersensitivity reactions, and peripheral neuropathy. Paclitaxel can cause infusion-related anaphylaxis; therefore, pre-medication and monitoring during infusion are critical. Hepatic dysfunction increases risk for toxicity, and caution is required in patients with compromised liver function. Paclitaxel is contraindicated in patients with a history of severe hypersensitivity to the drug or its excipients.
Precautions
Patients should be monitored for bone marrow suppression, liver function abnormalities, and neuropathy. Concomitant use with other myelosuppressive agents increases the risk of hematologic toxicity. Paclitaxel is metabolized via CYP2C8 and CYP3A4 pathways; co-administration with strong inhibitors or inducers may alter drug exposure. Adequate hydration and monitoring for fluid retention are recommended. Pregnancy and breastfeeding are contraindicated due to teratogenic potential.
Expert Tips
Ensure pre-medication to prevent hypersensitivity reactions and maintain strict infusion protocols. Monitor blood counts and liver function regularly. Educate patients about signs of neuropathy, infection, and infusion reactions. Pharmacists should counsel on proper preparation, handling, and disposal, particularly for cytotoxic drugs. Coordination with oncology teams is essential for combination regimens and supportive care planning.