Panitumumab
Overview
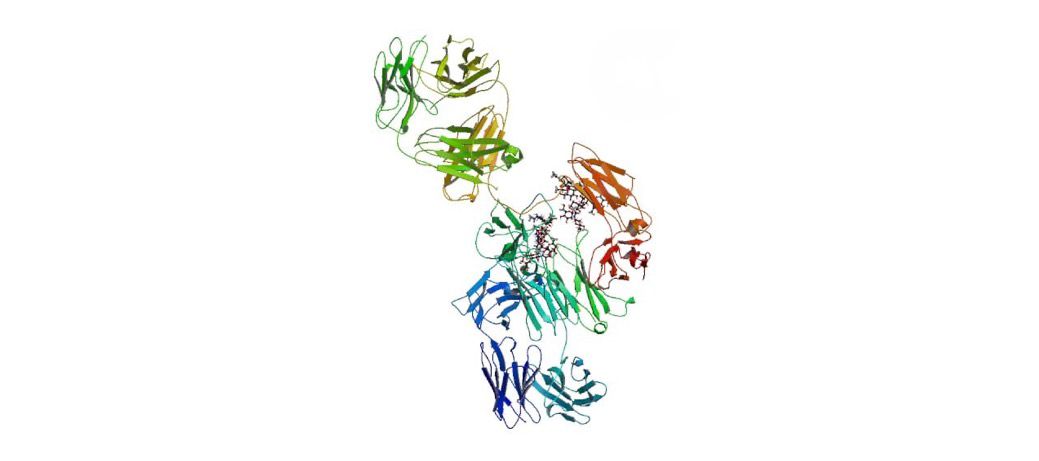
Panitumumab is a fully human IgG2 monoclonal antibody that targets the epidermal growth factor receptor (EGFR), a key driver of cell proliferation in certain cancers. By binding to EGFR, Panitumumab prevents the receptor from activating downstream signaling pathways that promote tumor growth and survival. This agent is specifically used to treat metastatic colorectal cancer in patients whose tumors have wild-type RAS genes (KRAS and NRAS). It may be given alone or in combination with chemotherapy regimens such as FOLFOX, offering a targeted immunotherapy approach that improves outcomes in selected patients.
Background and Date of Approval
Panitumumab was first approved by the U.S. Food and Drug Administration in September 2006 for the treatment of EGFR-expressing metastatic colorectal cancer in patients who have progressed after fluoropyrimidine, oxaliplatin, and irinotecan therapy. It was the first fully human anti-EGFR antibody to demonstrate that KRAS mutation status serves as a predictive biomarker. European approval followed in 2007, and numerous clinical trials including the PRIME and ASPECCT studies refined its use, confirming benefit only in RAS wild-type disease. In 2017, the FDA expanded approval for Panitumumab as first-line therapy combined with FOLFOX in RAS wild-type metastatic colorectal cancer. This established Panitumumab as a precision therapy built on molecular tumor profiling.
Uses
Panitumumab is indicated for adult patients with metastatic colorectal cancer that express EGFR and have confirmed wild-type RAS genes. It is used as monotherapy after disease progression on prior chemotherapy regimens and as first-line therapy when combined with FOLFOX in RAS wild-type tumors. Determination of KRAS and NRAS mutation status is mandatory before initiating therapy, as Panitumumab is not effective in patients with RAS mutations. This approach underscores the importance of molecular profiling in guiding therapeutic strategies and maximizing clinical benefit.
Administration
Panitumumab is administered by intravenous infusion every 14 days. The recommended dose is 6 mg per kilogram of body weight, delivered over 60 minutes for doses up to 1000 mg and over 90 minutes if the dose exceeds 1000 mg. Treatment continues until disease progression or unacceptable toxicity occurs. Close monitoring is required during infusion and throughout therapy to manage potential reactions and ensure patient safety.
Side Effects
The most frequently reported side effects of Panitumumab include a distinctive acne-like rash, dry skin, itching, paronychia, fatigue, nausea, diarrhea, and low levels of magnesium or potassium. These skin-related effects occur in nearly all patients and typically develop within the first few weeks of treatment. Though often manageable, severe skin reactions may necessitate therapy interruption.
Warnings
Serious adverse events may include dehydration due to severe diarrhea, low electrolyte levels, lung toxicity such as interstitial lung disease, and vision changes such as keratitis. Rare but potentially serious skin infections and nail complications may occur. Panitumumab can cause embryo-fetal toxicity and is contraindicated in pregnancy; effective contraception is required during treatment and for several months afterward. Certain skin toxicities correlate with improved outcomes, though they still require careful management. Patients should immediately report symptoms like severe rash, fever, or visual disturbances to their healthcare provider.
Precautions
Prior to starting Panitumumab, patients must undergo testing to confirm wild-type RAS status. Cardiac monitoring is generally not required, but close monitoring of serum electrolytes, especially magnesium and potassium, is recommended. As Panitumumab may increase photosensitivity, patients are advised to use sunscreen and avoid prolonged sun exposure during and after therapy. Co-administration with other EGFR inhibitors or immunosuppressives has not been well studied and should be done cautiously.
Expert Tips
When prescribing Panitumumab, ensure accuracy of RAS testing; prescribing without confirmation may result in ineffective therapy. Educate patients about the likelihood of skin reactions and provide prophylactic skincare strategies to reduce severity. Monitor hydration status and electrolyte levels, and consider early dermatologic referral for severe skin events. Pharmacists should review concurrent medications to avoid compounding risk for electrolyte disturbances or dehydration.
FAQs
What is Panitumumab?
How is Panitumumab given?
What are the common side effects?
Is Panitumumab safe in pregnancy?
How do I know if it will work?
References
1) https://www.medicines.org.uk/emc/files/pil.6178.pdf
2) https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125147s080lbl.pdf
3) https://www.ema.europa.eu/en/documents/product-information/vectibix-epar-product-information_en.pdf
4) https://www.pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/vectibix/vectibix_pi.pdf
