Peg L‑Asparaginase
Overview
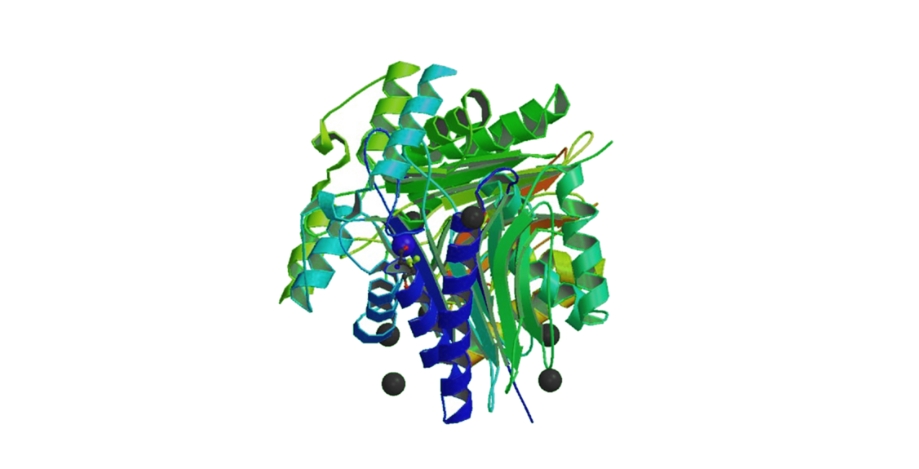
Peg L‑Asparaginase, commonly referred to as pegaspargase, is a pegylated form of the enzyme L‑asparaginase used as part of multi‑agent chemotherapy regimens for acute lymphoblastic leukemia (ALL). Pegylation involves attaching polyethylene glycol to the L‑asparaginase enzyme, which increases its circulating half‑life and reduces immunogenicity compared with native L‑asparaginase, allowing less frequent dosing. The therapeutic mechanism centers on depletion of circulating asparagine, an amino acid that leukemic cells cannot adequately synthesize, leading to inhibition of protein synthesis, cell cycle arrest, and leukemic cell death. Peg L‑Asparaginase is typically administered by intramuscular injection or intravenous infusion under clinical supervision, often in combination with agents such as vincristine, corticosteroids, and anthracyclines in structured frontline or relapse treatment protocols for pediatric and adult patients. Its improved pharmacokinetics and reduced hypersensitivity potential compared with earlier enzyme formulations have made pegaspargase an established component of ALL therapy in both pediatric and adult populations.
Background and Date of Approval
Peg L‑Asparaginase was originally approved by the United States Food and Drug Administration in 1994 for the treatment of acute lymphoblastic leukemia in patients who developed hypersensitivity to native L‑asparaginase preparations. In 2006, this approval was expanded to include first‑line use as part of multi‑agent chemotherapy regimens for ALL in pediatric and adult patients. Regulatory authorities in other regions, including the European Union, have granted marketing authorisations reflecting similar clinical indications. The approval history reflects its evolution from a specialist rescue therapy to a foundational enzyme component in ALL combination treatments, with pivotal clinical data demonstrating comparable or improved outcomes and tolerability relative to native L‑asparaginase formulations.
Uses
Peg L‑Asparaginase is indicated as a component of combination chemotherapy regimens for the treatment of acute lymphoblastic leukemia in pediatric and adult patients. It is used both as first‑line therapy for newly diagnosed ALL in multi‑agent protocols and as a treatment option for patients who have developed clinical hypersensitivity to native L‑asparaginase products. Implementation of pegaspargase therapy helps deplete asparagine, which leukemic cells require for survival, and is tailored to individual treatment phases such as induction, consolidation, or intensification within established ALL protocols.
Administration
Peg L‑Asparaginase is administered by intramuscular injection or intravenous infusion, typically as a single dose of approximately 2,500 international units per square meter of body surface area, with administration intervals no more frequent than every 14 days as part of structured chemotherapy cycles. Dosing intervals and routes are determined based on treatment phase, age, concomitant agents, and clinical response. Adults with ALL may receive adjusted dosing based on clinical factors and enzyme activity monitoring. Baseline and ongoing assessments including liver function tests, pancreatic enzymes, coagulation profiles, and complete blood counts are essential to guide dose adjustments and monitor safety.
Side Effects
Common side effects observed with Peg L‑Asparaginase therapy include elevation of liver transaminases, hypoalbuminemia, febrile neutropenia, hypertriglyceridemia, hyperglycemia, increased bilirubin, pancreatitis, nausea, vomiting, abdominal discomfort, injection site reactions, fatigue, and metabolic disturbances. The frequency and severity of these effects vary among patients and are influenced by concurrent chemotherapy and individual susceptibility. Careful monitoring and supportive care help manage these adverse effects during treatment.
Warnings
Serious adverse events associated with Peg L‑Asparaginase include severe hypersensitivity reactions and anaphylaxis, significant coagulopathy including thrombosis and bleeding abnormalities, severe pancreatitis, hepatotoxicity with liver dysfunction, hyperglycemia, severe neutropenia with associated infections, and metabolic disturbances. The risk of serious thrombotic events and clotting disorders necessitates vigilant clinical surveillance. Peg L‑Asparaginase is contraindicated in patients with a history of life‑threatening hypersensitivity to this drug or severe hepatic impairment. Clinicians should be prepared to manage acute hypersensitivity reactions and complications promptly.
Precautions
Prior to initiating Peg L‑Asparaginase therapy, baseline evaluation should include complete blood counts, liver and renal function tests, coagulation studies, and assessment for prior hypersensitivity to asparaginase products. Caution is warranted in patients with pre‑existing liver disease, pancreatitis, coagulopathies, or a history of thrombosis. Concomitant use of other hepatotoxic or anticoagulant medications may increase the potential for adverse effects and warrants careful clinical consideration. Live vaccines should generally be avoided during significant immunosuppression. Regular clinical follow‑up is essential to detect and manage toxicities early.
Expert Tips
Appropriate patient selection for Peg L‑Asparaginase includes confirming ALL diagnosis, evaluating for prior asparaginase hypersensitivity, and assessing baseline organ function. Monitoring should include serial liver function tests, pancreatic enzymes, coagulation profiles, and complete blood counts before each dose and throughout therapy. Patients should be counselled on recognizing signs of severe hypersensitivity, pancreatitis, thrombosis, bleeding, and infection, and advised to seek immediate medical care if symptoms arise. Premedication strategies and careful administration technique may reduce infusion‑related reactions. Coordination with supportive care, metabolic monitoring, and growth factor support can improve tolerability and maintain continuity of chemotherapy protocols.
