Pembrolizumab
Overview
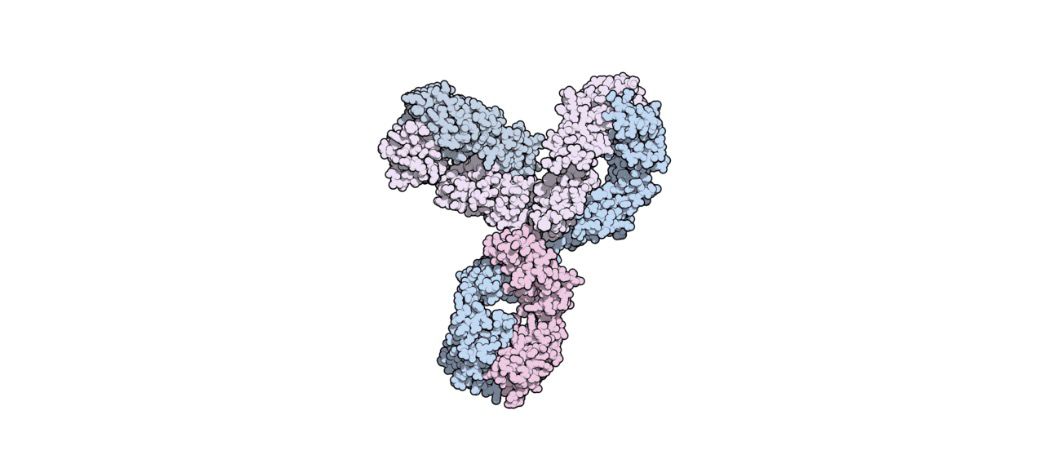
Pembrolizumab is a humanized monoclonal antibody that binds to the programmed death‑1 (PD‑1) receptor on T-cells. By blocking PD‑1, pembrolizumab lifts inhibitory signals that suppress immune response, enabling T cells to recognise and destroy cancer cells more effectively. Given via intravenous infusion, pembrolizumab is a form of immunotherapy rather than traditional cytotoxic chemotherapy. Its mechanism leverages the patient’s own immune system, making it effective across multiple cancer types, especially where tumor characteristics allow immune activation.
Background and Date of Approval
Pembrolizumab was first approved by the U.S. Food and Drug Administration in September 2014 for patients with unresectable or metastatic melanoma following prior therapy. In October 2015, FDA expanded its approval to include metastatic non‑small cell lung cancer (NSCLC) whose tumors express PD‑L1 and have progressed after platinum-based chemotherapy. On October 24, 2016, FDA granted first-line approval of pembrolizumab for metastatic NSCLC with high PD‑L1 expression in patients without EGFR or ALK mutations. Over the years, regulatory approvals have expanded to many cancer types worldwide, making pembrolizumab a cornerstone in cancer immunotherapy.
Uses
Pembrolizumab is indicated for treatment of various advanced or metastatic cancers. This includes unresectable or metastatic melanoma, metastatic non‑small cell lung cancer (NSCLC) as monotherapy or with chemotherapy depending on tumor PD‑L1 status and prior treatment, head and neck squamous cell carcinoma, and other cancers where regulatory approval exists. Use may be as monotherapy or in combination regimens, depending on cancer type, line of therapy, and patient’s molecular/tumor characteristics.
Administration
Pembrolizumab is administered intravenously, typically as a 30-minute infusion. A common adult dose is 200 mg every three weeks. In some regimens or indications, alternate dosing such as 400 mg every six weeks may be used depending on prescribing information and clinical judgment. Treatment usually continues until disease progression, unacceptable toxicity, or a predefined duration based on indication and protocol. Prior to therapy initiation, baseline organ function and relevant biomarker status should be assessed; periodic monitoring is advised during therapy.
Side Effects
Commonly reported side effects include fatigue, decreased appetite, nausea, cough, dyspnea, diarrhea or constipation, skin rash or itching, musculoskeletal pain, and general weakness. Because pembrolizumab modulates immune response, immune-related side effects affecting various organ systems are also common and require vigilance.
Warnings
Serious risks with pembrolizumab stem from immune-mediated toxicities. These may include pneumonitis, colitis, hepatitis, endocrinopathies such as thyroid dysfunction or adrenal insufficiency, nephritis, and skin toxicity. These adverse events can be severe or life-threatening, requiring prompt recognition, discontinuation of therapy, and immunosuppressive treatment when indicated. Patients with pre-existing autoimmune diseases or compromised organ function need careful evaluation before initiation.
Precautions
Before starting pembrolizumab, baseline assessment of organ function is essential. Use with other immunosuppressive agents or concurrent serious illness may affect risk/benefit balance. Live vaccines are generally contraindicated during therapy. Pembrolizumab is a monoclonal antibody and is not metabolized through typical drug pathways, so classical drug-drug interactions are uncommon, but any therapy that affects immune response should be used cautiously. Continuous monitoring for new symptoms, especially respiratory, gastrointestinal, endocrine, or renal, is critical during treatment.
Expert Tips
Counsel patients thoroughly about the mechanism of action, possible immune-related side effects, and the importance of reporting any new or worsening symptoms promptly. Obtain baseline labs for liver, kidney, pulmonary, and endocrine function. Schedule regular follow-ups to detect early signs of immune toxicity. Ensure infusion protocols and storage conditions are followed strictly. When combining with chemotherapy or other agents, coordinate schedules carefully and monitor for additive toxicity.
FAQs
What is pembrolizumab?
How is pembrolizumab administered?
What cancers is pembrolizumab used for?
What are common side effects of pembrolizumab?
What serious risks are associated with pembrolizumab?
How long is pembrolizumab treatment continued?
What monitoring is required during therapy with pembrolizumab?
References
1) https://www.ema.europa.eu/en/documents/procedural-steps-after/keytruda-epar-procedural-steps-taken-scientific-information-after-authorisation_en.pdf
2) https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/125514s128lbl.pdf
3) https://www.nccn.org/search-result?indexCatalogue=nccn-search-index&searchQuery=pembrolizunab
