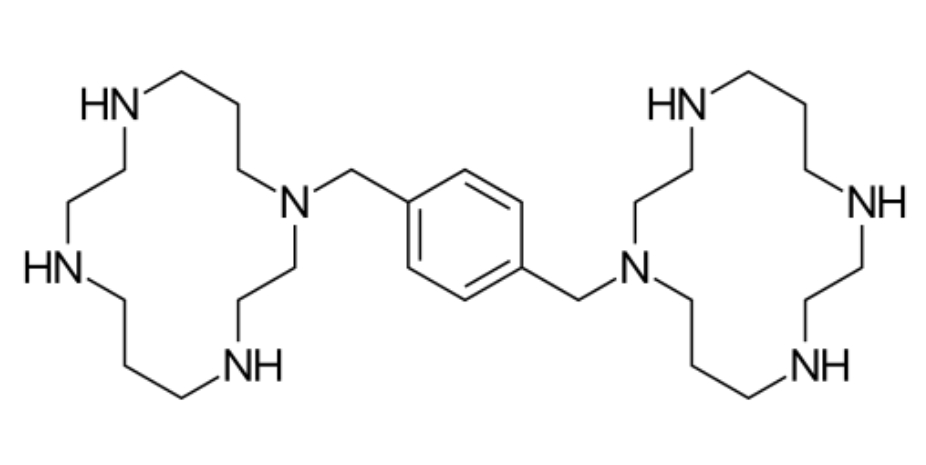
Plerixafor
Overview
Plerixafor is a small‑molecule antagonist of the C‑X‑C chemokine receptor type 4 (CXCR4) that promotes mobilization of hematopoietic stem cells (HSCs) from the bone marrow into peripheral blood. The interaction between CXCR4 on stem cells and its ligand stromal cell‑derived factor‑1 (SDF‑1) in the bone marrow microenvironment normally helps retain these cells within marrow. By inhibiting this interaction, plerixafor facilitates release of CD34‑positive stem cells into the bloodstream, where they can be collected by apheresis and stored for later reinfusion in autologous stem cell transplantation procedures. Because its mechanism does not directly kill cancer cells but rather enhances stem cell harvest, plerixafor is used in conjunction with a granulocyte‑colony stimulating factor to improve yields of stem cells for transplant in patients with hematologic malignancies who may mobilize poorly with growth factor alone. The drug’s targeted mode of action and predictable pharmacologic effects have made it an important supportive care agent in stem cell transplant protocols.
Background and Date of Approval
Plerixafor was first approved by the United States Food and Drug Administration on December 15, 2008 for use in combination with granulocyte‑colony stimulating factor to mobilize hematopoietic stem cells to the peripheral blood for collection prior to autologous transplantation in patients with non‑Hodgkin’s lymphoma and multiple myeloma. Subsequent regulatory reviews in the European Union and other regions led to similar marketing authorisations, reflecting its role in enhancing stem cell harvest in defined clinical settings. Plerixafor has orphan drug designation in both the United States and the European Union for stem cell mobilization, underscoring its specific use in transplant preparation.
Uses
Plerixafor is indicated in adult patients with non‑Hodgkin’s lymphoma or multiple myeloma who are undergoing autologous hematopoietic stem cell transplantation, when given in combination with a granulocyte‑colony stimulating factor to mobilize HSCs into peripheral blood for collection by apheresis. It is typically used in patients who are expected to mobilize poorly with granulocyte‑colony stimulating factor alone or after chemotherapy. The indication focuses on achieving adequate CD34‑positive cell counts to support engraftment following high‑dose chemotherapy and transplant.
Administration
Plerixafor is administered by subcutaneous injection, generally in the evening on days when stem cell mobilization is desired, usually in conjunction with daily granulocyte‑colony stimulating factor. The common dosing regimen is based on weight, often approximately 0.24 milligrams per kilogram of body weight administered once per day, typically for two to four days, with injections given about 10 to 11 hours prior to planned apheresis sessions. Baseline clinical and laboratory assessment are used to guide dosing schedules and adjust treatment based on response. Frequent monitoring of CD34‑positive cell counts helps determine timing of apheresis after plerixafor administration.
Side Effects
Common side effects observed with plerixafor include gastrointestinal symptoms such as nausea and diarrhea, injection site reactions, headache, dizziness, fatigue, arthralgia, and vomiting. These effects vary in severity and frequency among patients, and most are mild to moderate, manageable with supportive care and clinical assessment.
Warnings
Serious adverse events associated with plerixafor include hypersensitivity reactions, including anaphylaxis and serious allergic responses, which can be life‑threatening if not managed immediately. Splenic enlargement has been noted in patients receiving plerixafor, and rare cases of splenic rupture have been reported, necessitating careful clinical evaluation and monitoring. Due to its pharmacologic effects, mobilization of malignant cells into circulation is a theoretical concern, particularly in some leukemias, and clinical monitoring is essential. Severe hematologic effects, including leukocytosis and alterations in platelet counts, also require careful observation. Plerixafor is contraindicated in patients with known hypersensitivity to the drug.
Precautions
Prior to initiating plerixafor therapy, baseline complete blood counts, liver and kidney function tests, and assessment for hypersensitivity history are necessary. Special caution is advised in patients with pre‑existing splenic disorders, significant hematologic abnormalities, or conditions that may predispose to bleeding or splenic rupture. Plerixafor has no major classic drug interactions but combined use with granulocyte‑colony stimulating factors should follow established transplant mobilization protocols. Live vaccines should generally be avoided during periods of significant immunosuppression. Regular clinical follow‑up and laboratory monitoring are essential to detect and manage toxicities early.
Expert Tips
Selecting appropriate patients for plerixafor therapy involves identifying those at risk for poor stem cell mobilization and ensuring they are candidates for autologous transplantation with growth factor support. Baseline and ongoing monitoring of CD34‑positive cell counts and complete blood counts guides stem cell harvest timing and safety. Patients should be counselled on potential signs of hypersensitivity, splenic discomfort, and hematologic changes requiring prompt medical attention. Administration should occur in a controlled clinical setting with staff trained to manage acute hypersensitivity. Coordination with transplant teams for scheduling apheresis sessions and supporting lab assessments improves outcomes.