Ranibizumab
Overview
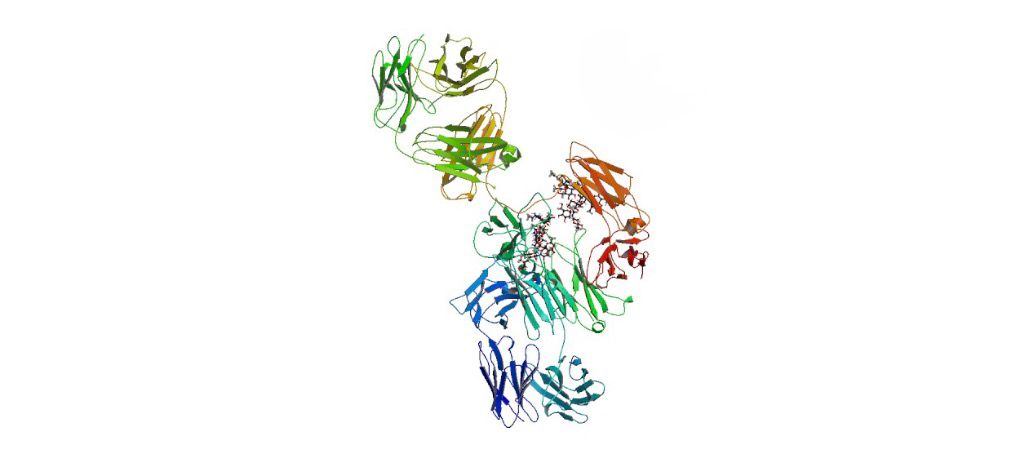
Ranibizumab is a recombinant humanized monoclonal antibody fragment that binds to vascular endothelial growth factor A (VEGF-A), inhibiting abnormal blood vessel growth and vascular leakage in the retina. It is primarily used for neovascular (wet) age-related macular degeneration (AMD), diabetic macular edema (DME), and macular edema following retinal vein occlusion (RVO). By neutralizing VEGF-A, Ranibizumab stabilizes or improves vision and prevents disease progression. Administered via intravitreal injection, it demonstrates rapid onset of action and has become a cornerstone in the management of retinal vascular diseases. Its favorable safety profile and efficacy in preserving visual acuity have established Ranibizumab as a leading anti-VEGF therapy worldwide.
Background and Date of Approval
Ranibizumab was developed as a fragment of the bevacizumab antibody to specifically target VEGF-A in ocular tissues. It received U.S. FDA approval in 2006 for neovascular AMD based on pivotal MARINA and ANCHOR trials, which demonstrated significant improvements in visual acuity compared to placebo or verteporfin photodynamic therapy. Subsequent approvals expanded indications to include DME, macular edema following RVO, and myopic choroidal neovascularization. The European Medicines Agency approved Ranibizumab for similar indications shortly thereafter. Its approval marked a transformative milestone in ophthalmology by offering an effective pharmacologic option to prevent vision loss in a range of retinal vascular disorders.
Uses
Ranibizumab is indicated for neovascular (wet) AMD, DME, macular edema secondary to RVO, and choroidal neovascularization associated with pathologic myopia. In neovascular AMD, it is used to maintain or improve visual acuity and reduce lesion progression. In DME, it is indicated to improve vision in adults with diabetic retinopathy and macular edema. Ranibizumab may be administered monthly or as needed (pro re nata) based on retinal response and optical coherence tomography (OCT) monitoring. Its efficacy in combination with other ocular interventions is supported in selected cases but is primarily used as monotherapy.
Administration
Ranibizumab is administered by intravitreal injection, usually in a sterile clinical setting. Standard dosing for neovascular AMD is 0.5 mg once monthly for three initial doses, followed by monthly or individualized dosing based on disease activity. For DME, macular edema following RVO, and myopic CNV, dosing regimens vary, but monthly injections with OCT-guided monitoring are standard. Patients require routine ophthalmologic evaluations, including visual acuity assessment and retinal imaging, to guide ongoing treatment and monitor for complications.
Side Effects
Frequent side effects include transient ocular discomfort, conjunctival hemorrhage, vitreous floaters, and increased intraocular pressure. Mild inflammation of the eye, such as iritis or uveitis, may occur. Systemic adverse effects are rare but include headache and mild flu-like symptoms. Most reactions are mild to moderate and resolve without intervention.
Warnings
Serious risks include endophthalmitis, retinal detachment, vitreous hemorrhage, and intraocular inflammation, which can threaten vision if untreated. Cases of thromboembolic events, including stroke and myocardial infarction, have been reported but are uncommon. Patients should seek immediate medical attention for eye pain, sudden vision loss, or floaters. Ranibizumab is contraindicated in patients with active ocular or periocular infections and known hypersensitivity to the drug or its components.
Precautions
Before initiating Ranibizumab, evaluate for active ocular infection or inflammation. Monitor intraocular pressure, lens status, and retinal integrity. No significant drug–drug interactions have been identified; however, concurrent anti-VEGF therapies should be avoided unless recommended by a specialist. Patients with cardiovascular comorbidities should be monitored for thromboembolic events, although risk is low.
Expert Tips
Ensure proper aseptic technique during intravitreal injections to minimize infection risk. Educate patients on post-injection care and signs of complications, such as eye pain, redness, or sudden vision changes. Visual acuity and OCT imaging should guide dosing intervals to balance efficacy and safety. Pharmacists can counsel on storage, handling, and proper disposal of single-use vials. Coordination with retina specialists is essential for optimal treatment planning and long-term monitoring.
