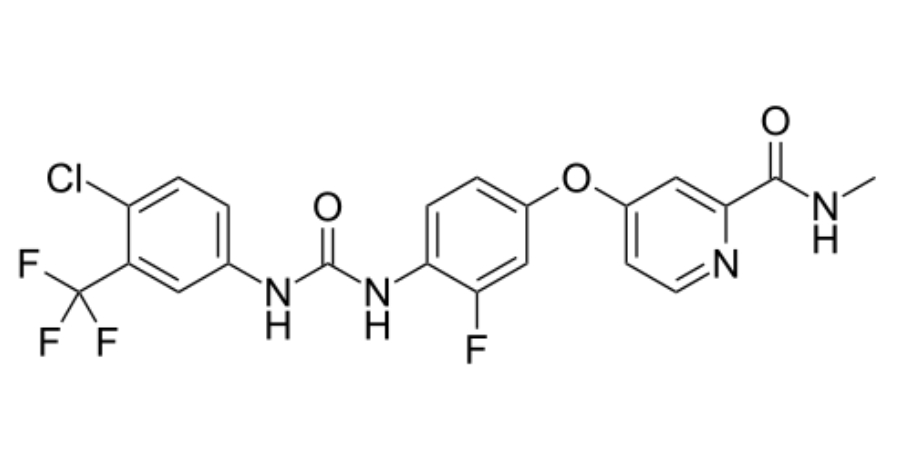
Regorafenib
Overview
Regorafenib is an orally administered small‑molecule targeted therapy belonging to the class of multi‑kinase inhibitors that block multiple protein kinases involved in tumor angiogenesis, oncogenesis, and the tumor microenvironment. It inhibits vascular endothelial growth factor receptors, platelet‑derived growth factor receptors, fibroblast growth factor receptors, and tyrosine kinases such as KIT, RET, and RAF‑1 that support cancer cell proliferation, survival, and spread. By interfering with these signaling pathways, regorafenib inhibits tumor growth, reduces vascular supply to tumors, and can impede metastatic progression. It is administered orally in structured cycles and is used in adult patients with advanced solid tumors for whom standard therapies have been exhausted or are no longer effective. Regorafenib’s mechanism and broad kinase inhibition profile establish it as a valuable option in select cancers with limited treatment alternatives.
Background and Date of Approval
Regorafenib received initial approval from the United States Food and Drug Administration in 2012 as an oral oncology therapy for specific advanced cancers. Its indication has since expanded; notably, in 2017, the FDA approved regorafenib for the treatment of hepatocellular carcinoma in patients previously treated with sorafenib, based on evidence demonstrating survival benefit in this population. Regulatory authorities in the European Union and other regions have likewise authorized regorafenib for similar advanced cancer indications including metastatic colorectal cancer and gastrointestinal stromal tumors after failure of prior therapies. These approvals reflect evidence from randomized clinical trials showing improved outcomes in patients with limited treatment options.
Uses
Regorafenib is indicated as monotherapy for adult patients with metastatic colorectal cancer who have received prior fluoropyrimidine‑, oxaliplatin‑, and irinotecan‑based chemotherapy regimens, anti‑angiogenic therapy, and for RAS wild‑type tumors an anti‑epidermal growth factor receptor therapy. It is also indicated for adult patients with locally advanced, unresectable, or metastatic gastrointestinal stromal tumors who have previously been treated with imatinib and sunitinib. Additionally, regorafenib is indicated for hepatocellular carcinoma in patients previously treated with sorafenib. Its use is tailored to patients with advanced disease and prior treatment failure, forming part of later‑line systemic therapy.
Administration
Regorafenib is administered by mouth as tablets. The recommended starting dose for adults is 160 milligrams once daily, typically given on days 1 through 21 of a 28‑day treatment cycle, and continued until disease progression or unacceptable toxicity occurs. Patients are advised to take regorafenib with water after a low‑fat meal at approximately the same time each day. Dose modifications, interruptions, or reductions in 40‑milligram increments may be necessary based on individual tolerability, adverse effects, and liver function status. Ongoing clinical and laboratory assessments including blood counts and liver tests guide safe dosing.
Side Effects
Common side effects of regorafenib include hand‑foot skin reaction, fatigue or asthenia, diarrhea, decreased appetite, hypertension, nausea, weight loss, rash, and abdominal pain. These effects vary in severity and frequency among patients and often require supportive care measures or dose adjustments to alleviate symptoms during treatment cycles.
Warnings
Serious adverse events associated with regorafenib include hepatotoxicity, which can be severe or fatal, necessitating close monitoring of liver function before and during treatment. Other serious toxicities include gastrointestinal perforation or fistula, severe hemorrhage, dermatologic toxicity including severe hand‑foot skin reactions, hypertension, cardiac ischemia or infarction, reversible posterior leukoencephalopathy syndrome, impaired wound healing, and severe infections. Permanent discontinuation is warranted in cases of life‑threatening hemorrhage, severe hypertension unresponsive to management, or other severe organ toxicities. Regorafenib is contraindicated in patients with known hypersensitivity to the drug or its components.
Precautions
Before initiating regorafenib therapy, baseline evaluations should include complete blood counts, liver and kidney function tests, blood pressure assessment, and evaluation of cardiovascular risk. Special caution is required in patients with significant hepatic impairment, bleeding disorders, or a history of cardiovascular disease. Regorafenib’s metabolism involves hepatic pathways, and concomitant use with strong CYP3A4 inducers or inhibitors may affect drug levels and toxicity, necessitating clinical judgment. Live vaccines should be avoided during treatment due to potential immunosuppression. Regular clinical and laboratory monitoring is essential to detect early signs of toxicity and adjust therapy accordingly.
Expert Tips
Selecting patients for regorafenib therapy involves confirming advanced disease status after appropriate prior treatments and assessing overall organ function to anticipate tolerability. Baseline and periodic monitoring of liver function, blood pressure, and dermatologic status can identify emerging toxicities early. Patients should be counseled on recognizing symptoms of severe side effects including persistent diarrhea, severe rash, abdominal pain, or signs of liver dysfunction. Administer regorafenib with meals to optimize absorption and adhere to dose modification guidelines for toxicity management. Coordination with multidisciplinary oncology care teams ensures timely dose adjustments, supportive care, and assessment of clinical response to maximize benefit while minimizing harm.
