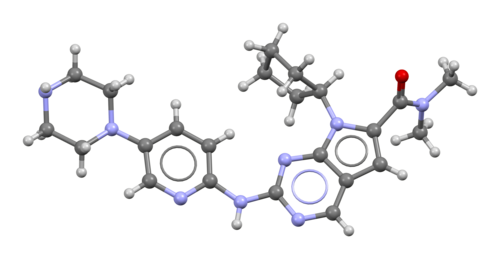
Ribociclib
Overview
Ribociclib is an orally active small molecule that selectively inhibits cyclin-dependent kinases 4 and 6, which are key regulators of cell cycle progression from the G1 phase to the S phase. By inhibiting CDK4 and CDK6 activity, ribociclib prevents phosphorylation of the retinoblastoma protein, leading to cell cycle arrest and suppression of cancer cell proliferation. It is classified as a targeted anticancer therapy and is primarily used in combination with endocrine therapies in hormone receptor-positive, human epidermal growth factor receptor 2-negative breast cancer. Ribociclib has demonstrated clinical importance in delaying disease progression and improving survival outcomes across multiple disease stages. The drug is administered orally in defined treatment cycles and requires regular monitoring due to its effects on hematologic parameters, liver function, and cardiac conduction.
Background and Date of Approval
Ribociclib was first approved by the United States Food and Drug Administration on March 13, 2017 for use in combination with an aromatase inhibitor as initial endocrine-based therapy for postmenopausal women with hormone receptor-positive, HER2-negative advanced or metastatic breast cancer. On July 18, 2018, the FDA expanded approval to include premenopausal and perimenopausal women, as well as use in combination with fulvestrant for patients with disease progression following endocrine therapy. On September 17, 2024, ribociclib received FDA approval for adjuvant treatment of adults with hormone receptor-positive, HER2-negative stage II and III early breast cancer at high risk of recurrence when used with an aromatase inhibitor. These approvals were supported by large phase III clinical trial programs demonstrating efficacy and manageable safety profiles.
Uses
Ribociclib is indicated for the treatment of hormone receptor-positive, HER2-negative advanced or metastatic breast cancer in combination with aromatase inhibitors or fulvestrant as initial therapy or following progression on endocrine therapy. It is also approved for adjuvant treatment of adults with high-risk hormone receptor-positive, HER2-negative early breast cancer when used with endocrine therapy. Ribociclib is used as part of combination regimens rather than as monotherapy and is prescribed based on disease stage, prior treatment history, and patient-specific clinical factors.
Administration
Ribociclib is administered orally, usually as 200 mg tablets taken once daily. The standard dosing regimen in advanced or metastatic disease is 600 mg daily for 21 consecutive days followed by 7 days off treatment, forming a 28-day cycle. In certain settings, including adjuvant therapy, a lower starting dose such as 400 mg daily for 21 days followed by 7 days off may be used according to approved protocols. Dose reductions to 400 mg or 200 mg may be required based on tolerability and laboratory findings. Ribociclib can be taken with or without food and should be taken at the same time each day. Treatment duration depends on disease response, toxicity, and clinical judgement.
Side Effects
Common side effects associated with ribociclib include neutropenia, leukopenia, infections, nausea, fatigue, diarrhea, vomiting, constipation, headache, alopecia, and elevations in liver enzymes. These effects are generally related to inhibition of cell cycle progression in rapidly dividing cells and vary in severity among patients. Most common adverse effects are manageable with dose adjustments, supportive care, and close medical supervision.
Warnings
Serious adverse events linked to ribociclib include severe neutropenia with increased risk of infection, hepatotoxicity, and QT interval prolongation, which may predispose to cardiac arrhythmias. Ribociclib should be used with caution in patients with pre-existing liver disease or cardiac conditions affecting electrical conduction. Regular monitoring is essential to detect serious toxicities early. Treatment interruption, dose reduction, or permanent discontinuation may be required if significant adverse events occur. Ribociclib may cause fetal harm, and pregnancy status should be assessed before initiation.
Precautions
Before starting ribociclib, baseline assessments should include complete blood counts, liver function tests, and evaluation of cardiac risk factors, including electrocardiography. Ongoing monitoring during treatment includes repeated blood counts, liver enzyme testing, and ECG assessments as clinically indicated. Ribociclib is metabolized via cytochrome P450 enzymes, and concomitant use of strong CYP3A inhibitors or inducers may significantly alter drug exposure, requiring dose modification or avoidance. Caution is advised when ribociclib is used alongside other agents that prolong the QT interval or cause overlapping toxicities.
Expert Tips
Careful patient selection is essential when prescribing ribociclib, with confirmation of hormone receptor-positive, HER2-negative disease status. Baseline laboratory and cardiac evaluations should be completed prior to initiation. Patients should be counselled on adherence to the dosing schedule, recognition of infection symptoms, and the importance of routine monitoring. Coordination with concurrent endocrine therapies requires attention to dosing schedules and management of combined side effects. Pharmacists should ensure appropriate dispensing, storage, and patient education to support safe and effective long-term therapy.
