Rituximab
Overview
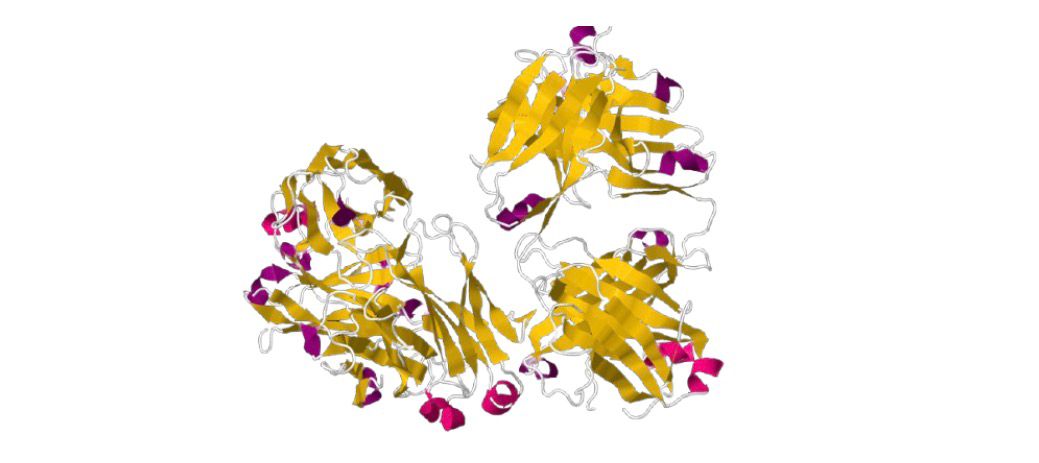
Rituximab is a chimeric monoclonal antibody targeting CD20 on B-lymphocytes. It is administered via intravenous infusion and is used to treat various B-cell malignancies and autoimmune disorders. Rituximab depletes CD20-positive B cells through mechanisms such as complement-dependent cytotoxicity and antibody-dependent cell-mediated cytotoxicity, helping reduce disease activity and tumor burden. It has broad applications in non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, vasculitis, and pemphigus vulgaris. Infusion-related reactions, immunosuppression, and risk of infection are key considerations. Regular monitoring during therapy is essential.
Background and Date of Approval
Rituximab was developed by IDEC and approved by the FDA in 1997 for B-cell non-Hodgkin lymphomas. Over time, its indications expanded to include chronic lymphocytic leukemia, rheumatoid arthritis with inadequate response to TNF antagonists, granulomatosis with polyangiitis, microscopic polyangiitis, and moderate to severe pemphigus vulgaris. The drug functions by binding CD20 on B cells and inducing their depletion via CDC and ADCC. Clinical experience shows sustained B-cell depletion lasting months.
Uses
Rituximab is used in multiple conditions: adult patients with non-Hodgkin’s lymphoma, as monotherapy or combined with chemotherapy; chronic lymphocytic leukemia in combination with fludarabine and cyclophosphamide; rheumatoid arthritis with methotrexate after failure of TNF antagonists; granulomatosis with polyangiitis and microscopic polyangiitis with glucocorticoids in patients aged 2 years and older; moderate to severe pemphigus vulgaris. Off-label use exists but should be clinically justified.
Administration
Rituximab is administered by intravenous infusion. Common regimens include: for chronic lymphocytic leukemia, 375 mg/m² before FC chemotherapy, then 500 mg/m² for cycles 2–6; for rheumatoid arthritis, two 1000 mg infusions separated by two weeks, repeated every 16–24 weeks; for granulomatosis with polyangiitis or microscopic polyangiitis, 375 mg/m² weekly for 4 weeks as induction, with maintenance dosing per protocol. Premedication with acetaminophen, antihistamines, and often glucocorticoids is required to reduce infusion reactions.
Side Effects
Frequently observed adverse effects include infusion-related reactions such as fever, chills, rash, itching, dyspnea, and hypotension. These typically occur during or shortly after infusion. Infections, fatigue, nausea, and cytopenias are also common. Monitoring and symptomatic management are advised. Patients experiencing severe or persistent symptoms should promptly contact their healthcare provider.
Warnings
Serious risks include fatal infusion-related reactions (especially during the first infusion), severe mucocutaneous reactions, hepatitis B reactivation, and progressive multifocal leukoencephalopathy. Hepatitis B screening is mandatory prior to initiation; positive patients should be managed according to guidelines. Monitor closely during infusions and discontinue rituximab if severe reactions occur.
Precautions
Rituximab induces prolonged B-cell depletion, increasing infection susceptibility. Live vaccines should be avoided; non-live vaccines should be completed at least four weeks before therapy. In patients with active infections or hepatitis B, rituximab is contraindicated or requires specialist consultation. Combination with other immunosuppressants may heighten risk of adverse effects.
Expert Tips
Ensure proper premedication to mitigate infusion reactions. Monitor vital signs during and after infusions, particularly in the first dose. Perform hepatitis B screening beforehand and consider prophylaxis or consultation if positive. Educate patients about symptoms of infection and infusion reactions and instruct immediate reporting. Coordinate with the multidisciplinary team when combining with chemotherapy or immunosuppressants.
