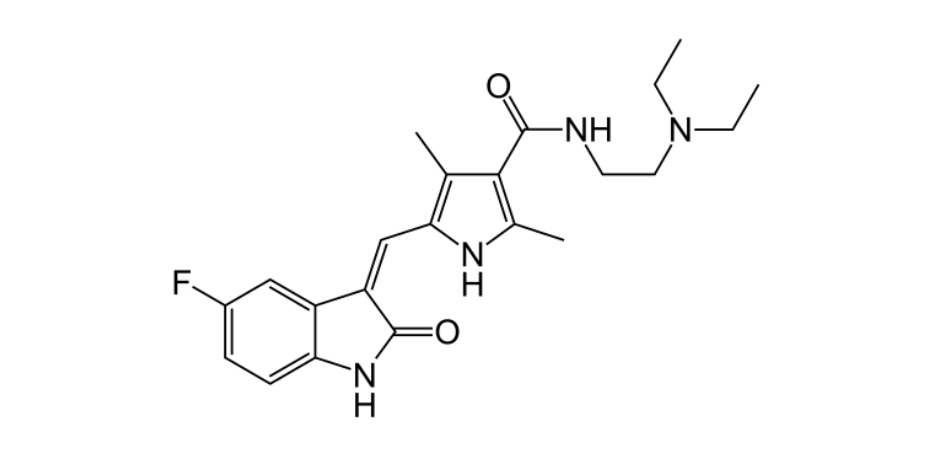
Sunitinib
Overview
Sunitinib is an orally administered small‑molecule multi‑targeted receptor tyrosine kinase inhibitor with antineoplastic and antiangiogenic properties. It blocks a range of kinases including vascular endothelial growth factor receptors, platelet‑derived growth factor receptors, KIT, and other signaling pathways that contribute to tumor cell proliferation, angiogenesis, and survival. By simultaneously inhibiting these targets, sunitinib reduces tumor vascular supply and impedes cancer progression in several solid tumors. Its oral route of administration and targeted mechanism make it an important option in oncology, particularly in patients with advanced disease who have limited alternatives. Sunitinib’s capacity to interfere with key growth and survival pathways in cancer cells underpins its role in prolonging progression‑free survival and delaying disease progression when used as indicated in multiple cancer types.
Background and Date of Approval
Sunitinib malate (brand name Sutent) received initial approval from the United States Food and Drug Administration on January 26, 2006 for the treatment of adult patients with gastrointestinal stromal tumor after disease progression on or intolerance to imatinib mesylate and for advanced renal cell carcinoma. Over subsequent years its regulatory profile expanded, including approval on May 20, 2011 for the treatment of progressive, well‑differentiated pancreatic neuroendocrine tumors in patients with unresectable locally advanced or metastatic disease, and on November 16, 2017 for the adjuvant treatment of adult patients at high risk of recurrent renal cell carcinoma following nephrectomy. In the European Union, sunitinib received conditional marketing authorization in July 2006 that was converted to full authorization in January 2007 for similar oncology indications. These sequential regulatory approvals reflect sunitinib’s established clinical benefit in several advanced solid tumors.
Uses
Sunitinib is indicated for the treatment of adult patients with gastrointestinal stromal tumor (GIST) after disease progression on or intolerance to imatinib, advanced renal cell carcinoma (RCC), progressive well‑differentiated pancreatic neuroendocrine tumors (pNET) that are unresectable or metastatic, and as adjuvant therapy for adult patients at high risk of recurrent RCC following nephrectomy. Its use is tailored to individuals with these specific cancer types and prior treatment history, representing both frontline and later‑line targeted therapy options in selected patients.
Administration
Sunitinib is administered orally in capsule form, typically at a dose of 50 milligrams once daily on a schedule of four weeks on treatment followed by two weeks off (4/2 schedule) for indications such as GIST and advanced RCC. For pancreatic neuroendocrine tumors, a continuous daily dosing regimen of 37.5 milligrams is commonly used. The adjuvant regimen for high‑risk post‑nephrectomy RCC also uses 50 milligrams once daily on the 4/2 schedule for up to nine cycles. Dosing should be individualized based on patient tolerance, adverse effects, and organ function, with clinical and laboratory monitoring guiding dose adjustments or interruptions.
Side Effects
Common side effects observed with sunitinib include fatigue or asthenia, diarrhea, nausea, mucositis or mouth sores, decreased appetite, vomiting, abdominal pain, hand‑foot skin reaction, hypertension, bleeding events, taste alterations, rash, and thrombocytopenia. These effects vary in frequency and severity among patients and often require supportive care or dose modification to manage during therapy.
Warnings
Serious adverse events associated with sunitinib include hepatotoxicity, which can be severe or fatal, cardiovascular events such as myocardial ischemia or heart failure, severe hemorrhage, gastrointestinal perforation, tumor lysis syndrome, thrombotic microangiopathy, and significant hematologic toxicities. Liver function should be monitored before and during treatment, and therapy modified or discontinued if severe toxicities occur. Sunitinib is contraindicated in patients with known hypersensitivity to the drug, and caution is warranted in those with pre‑existing cardiovascular or bleeding disorders.
Precautions
Prior to initiating sunitinib therapy, baseline evaluations should include complete blood counts, liver and kidney function tests, and cardiovascular assessment. Patients with significant hepatic impairment, uncontrolled hypertension, or bleeding diatheses require careful consideration. Sunitinib’s metabolism involves hepatic pathways, and caution is advised when co‑administering strong CYP3A4 inhibitors or inducers. Live vaccines should be avoided during treatment due to potential immune effects. Regular clinical monitoring and laboratory testing are essential to detect toxicity early and adjust therapy appropriately.
Expert Tips
Appropriate patient selection for sunitinib involves confirming the specific regulatory‑approved indication, prior therapy history, and comprehensive assessment of organ function. Baseline and periodic monitoring of liver enzymes, blood pressure, hematologic parameters, and signs of bleeding can help identify emerging toxicities. Patients should be counselled on recognizing symptoms of severe side effects such as persistent diarrhea, severe mucositis, or unexplained bruising. Administer sunitinib with or without food at the same time each day, and adhere to recommended dose modification strategies for toxicity management. Close coordination with multidisciplinary oncology care teams ensures timely dose adjustments, supportive care, and assessment of treatment response.
