Teriparatide
Overview
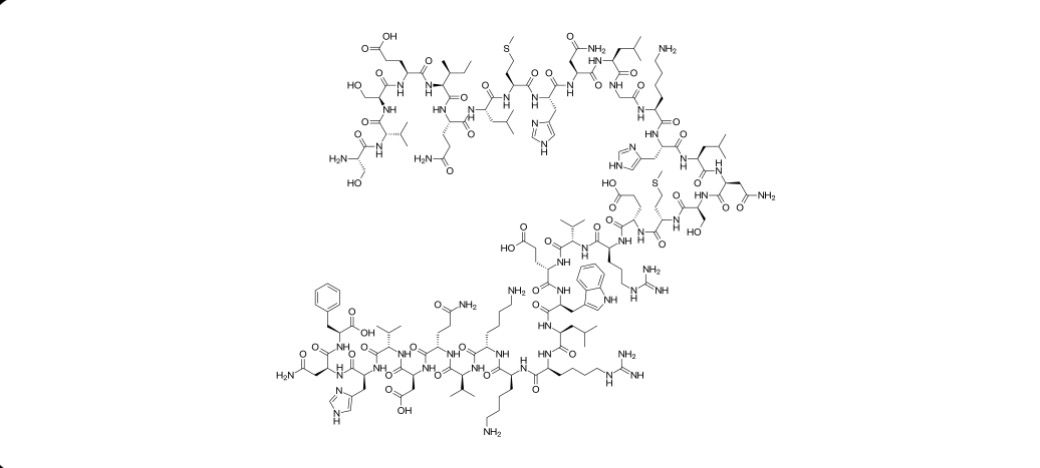
Teriparatide is a synthetic form of the amino‑terminal fragment of human parathyroid hormone that acts as a potent anabolic agent for bone. Unlike antiresorptive osteoporosis therapies that slow bone loss, teriparatide stimulates osteoblast function and promotes new bone formation, increasing bone mass and improving bone microarchitecture. When administered once daily by subcutaneous injection, intermittent exposure to teriparatide enhances trabecular and cortical bone formation, leading to increased bone mineral density and reduced risk of fragility fractures in patients with osteoporosis at high risk of fracture. This unique mechanism differentiates teriparatide from other osteoporosis treatments and supports its role in patients with severe disease or those who have failed or are intolerant to alternative therapies. Treatment is typically limited to a defined period due to its potent anabolic effect and clinical safety considerations.
Background and Date of Approval
Teriparatide was first approved by the United States Food and Drug Administration in 2002 under the brand name Forteo as the first bone anabolic agent for the treatment of osteoporosis. The initial FDA approval on 26 November 2002 established its use in postmenopausal women with osteoporosis at high risk for fracture. Subsequent regulatory approvals have expanded its use for increasing bone mass in men with primary or hypogonadal osteoporosis at high risk for fracture, and for the treatment of osteoporosis associated with sustained systemic glucocorticoid therapy in adults at high risk for fracture. Additional formulations and generic versions, including pen‑based delivery devices, have been approved in the United States and other regions thereafter. These approvals were based on pivotal clinical trials demonstrating significant reductions in vertebral and nonvertebral fracture risk and increases in bone mineral density with once‑daily dosing.
Uses
Teriparatide is indicated for the treatment of osteoporosis in adults at high risk for fractures. Approved indications include postmenopausal women with osteoporosis at high risk for fracture or who cannot use other available treatments, men with primary or hypogonadal osteoporosis at high risk for fracture or who cannot use other treatments, and men and women with osteoporosis associated with sustained systemic glucocorticoid therapy who are at high risk for fracture or unable to use other therapies. These indications reflect teriparatide’s anabolic mechanism, which is distinct from antiresorptive agents, making it particularly useful when rapid bone formation is clinically desirable.
Administration
Teriparatide is administered by subcutaneous injection, usually in the thigh or abdomen, once daily at a dose of 20 micrograms. The injection should be given at approximately the same time each day and does not require adjustment for age or gender under usual conditions. Patients should be instructed on proper injection technique and advised to rotate injection sites to minimise local reactions. Calcium and vitamin D supplementation are recommended if dietary intake is inadequate. Treatment with teriparatide is generally limited to a total duration of up to 24 months over a patient’s lifetime, and continuation beyond this period should be considered only if fracture risk remains high after careful clinical assessment.
Side Effects
Common side effects of teriparatide include nausea, headache, dizziness, leg cramps, and injection site reactions such as pain or redness. Patients may also experience mild increases in serum calcium concentrations soon after dosing. These effects vary between individuals and are generally transient or manageable with clinical supervision and supportive care. Monitoring of serum calcium and patient symptoms is recommended during therapy to identify and address common adverse responses.
Warnings
Serious adverse events include orthostatic hypotension, especially after the first few doses, which may increase the risk of falls in susceptible individuals. There is a theoretical concern for osteosarcoma associated with teriparatide observed in animal studies, and although human data have not conclusively demonstrated a significant risk, teriparatide should be avoided in patients with predisposing conditions for osteosarcoma such as Paget disease of bone, prior external beam radiation involving the skeleton, or hereditary skeletal malignancies. Teriparatide is contraindicated in patients at increased baseline risk of osteosarcoma and those with unexplained elevated alkaline phosphatase of skeletal origin. Use should be avoided in conditions with excessive baseline calcium levels or other metabolic bone disorders not related to osteoporosis.
Precautions
Prior to initiating teriparatide, a baseline assessment of bone mineral density, serum calcium, and renal function should be performed. Patients with hyperparathyroidism, severe renal impairment, or high baseline serum calcium levels require careful evaluation before therapy. Concurrent use of medications that affect calcium metabolism, such as digoxin, may require careful monitoring due to potential interactions with teriparatide’s effects on calcium balance. Patients should be counselled on symptoms of hypercalcemia, such as fatigue, nausea, or increased thirst, and advised to report these promptly.
Expert Tips
When prescribing teriparatide, individualise therapy based on fracture risk, prior treatment history, and bone density measurements. Educate patients on correct subcutaneous injection technique, timing of doses, and the importance of calcium and vitamin D supplementation if needed. Provide guidance on recognising signs of orthostatic hypotension and hypercalcemia. Regular monitoring of serum calcium and renal function supports safe long‑term use. After completing the maximal recommended duration of therapy, transition patients to antiresorptive agents to help preserve gains in bone density.
