Tislelizumab
Overview
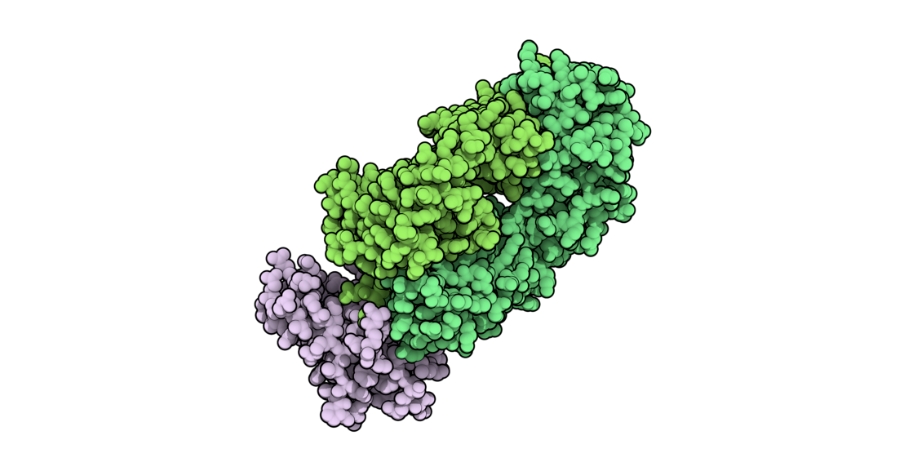
Tislelizumab is a recombinant humanized immunoglobulin G4 monoclonal antibody that targets the programmed cell death protein‑1 (PD‑1) receptor on activated T lymphocytes. By binding to PD‑1, tislelizumab blocks the interaction between PD‑1 and its ligands, PD‑L1 and PD‑L2, which are often upregulated on tumor cells and within the tumor microenvironment to suppress immune surveillance. This blockade restores antitumor immune responses by enabling T cells to recognize and destroy cancer cells. Tislelizumab is engineered with modifications that minimize binding to Fc gamma receptors on macrophages, which may reduce antibody‑dependent cellular phagocytosis and enhance its immune‑activating potential relative to some other PD‑1 inhibitors. It is administered intravenously under clinical supervision, typically in combination with chemotherapy or as monotherapy depending on the cancer type and treatment setting. Its role as an immune checkpoint inhibitor places it at the forefront of modern immunotherapies for solid tumors and certain hematologic malignancies, expanding treatment options for patients with advanced disease.
Background and Date of Approval
Tislelizumab was first approved for medical use in China in December 2019 for the treatment of patients with relapsed or refractory classical Hodgkin’s lymphoma after at least second‑line chemotherapy. Subsequent approvals in China have included metastatic urothelial carcinoma with high PD‑L1 expression, non‑small cell lung cancer in combination with chemotherapy, and hepatocellular carcinoma as monotherapy. In 2023 the European Union granted marketing authorization for tislelizumab in selected cancer indications, and in March 2024 the United States Food and Drug Administration approved tislelizumab‑jsgr for the treatment of adult patients with unresectable or metastatic esophageal squamous cell carcinoma after prior chemotherapy. Other regional approvals, including in Australia in 2024, reflect its expanding global regulatory footprint. These approvals are supported by pivotal clinical trials demonstrating improved outcomes in defined patient populations with advanced solid tumors and hematologic malignancies.
Uses
Tislelizumab is indicated for the treatment of adult patients with unresectable or metastatic esophageal squamous cell carcinoma after prior systemic chemotherapy. It is also approved in various regions for additional oncology indications including, in combination with platinum‑based chemotherapy, first‑line treatment of certain non‑small cell lung cancers with PD‑L1 expression, and as monotherapy or in combination regimens for hepatocellular carcinoma, urothelial carcinoma, and classical Hodgkin’s lymphoma. Indications may vary by country and regulatory authority, and use is tailored to tumor type, prior therapy, and biomarker status.
Administration
Tislelizumab is administered by intravenous infusion, typically as 200 milligrams given over approximately 60 minutes once every three weeks. This schedule continues until disease progression or unacceptable toxicity. Dose modifications, interruptions, or discontinuation may be required based on individual patient tolerability and the occurrence of immune‑related adverse events. Infusion should be performed in a clinical setting with appropriate monitoring for infusion‑related reactions. Baseline evaluations and ongoing assessments are used to guide treatment decisions and adjust therapy based on clinical response and safety.
Side Effects
Commonly observed side effects with tislelizumab include fatigue, anemia, decreased neutrophil count, nausea, diarrhea, rash, pruritus, and infusion‑related reactions. The frequency and severity of these effects vary among patients and may be influenced by combination with chemotherapy or other systemic therapies. Many side effects are manageable with supportive care and clinical monitoring.
Warnings
Serious adverse events associated with tislelizumab are characteristic of immune checkpoint inhibitors and include immune‑mediated toxicities such as pneumonitis, colitis, hepatitis, endocrinopathies including thyroiditis and adrenal insufficiency, nephritis, and severe dermatologic reactions. Fatal events have been reported due to respiratory failure or severe hepatic injury in rare cases. Infusion‑related reactions, severe infections, and exacerbation of underlying autoimmune disorders have also occurred. Tislelizumab should be used with caution in patients with pre‑existing autoimmune conditions and is contraindicated in those with a history of severe hypersensitivity to the drug. Prompt recognition and management of immune‑related adverse events are essential to prevent serious outcomes.
Precautions
Before initiating tislelizumab therapy, baseline assessments should include complete blood counts, liver and kidney function tests, thyroid function, and evaluation for pre‑existing autoimmune disease. Special caution is warranted in patients with significant organ dysfunction, chronic infections, or a history of immune‑mediated conditions. Concomitant administration of live vaccines should be avoided during and after treatment due to the risk of uncontrolled infection. There are no major classic pharmacokinetic drug interactions identified; however, combined use with other immunosuppressive agents requires careful clinical judgement. Regular clinical and laboratory monitoring is essential to detect early signs of immune‑related adverse events and to guide management.
Expert Tips
Appropriate patient selection for tislelizumab involves confirming a regulatory‑approved indication based on tumor type, prior therapy, and relevant biomarkers such as PD‑L1 expression where applicable. Baseline and periodic monitoring of organ function, blood counts, and endocrine parameters helps identify emerging toxicities. Patients should be counselled on the importance of reporting symptoms suggestive of immune‑related adverse events, including respiratory symptoms, severe diarrhea, skin changes, or fatigue. Premedication is generally not required but readiness to manage infusion‑related reactions is advised. Coordination with multidisciplinary oncology teams fosters comprehensive care, ensuring timely dose adjustments, supportive care interventions, and evaluation of therapeutic response.
