Tocilizumab
Overview
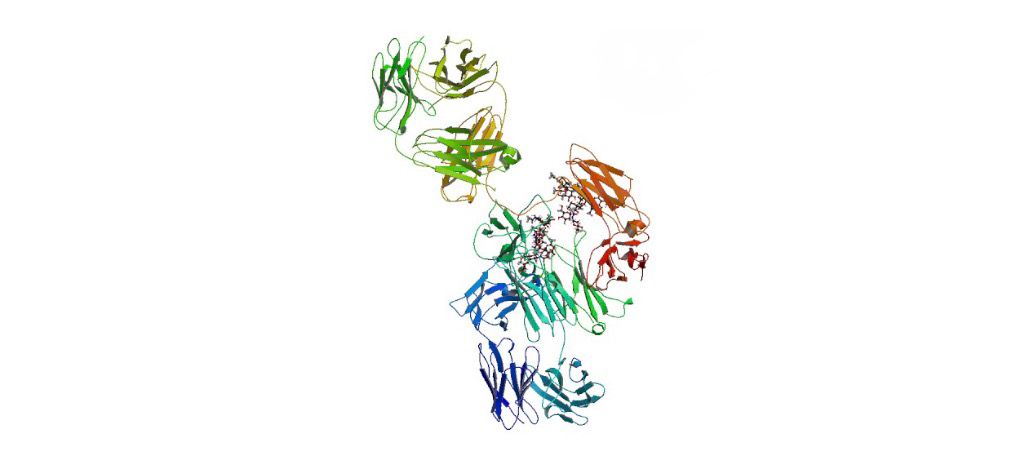
Tocilizumab is a humanized immunoglobulin G1 monoclonal antibody that binds to both soluble and membrane‑bound interleukin‑6 (IL‑6) receptors, preventing IL‑6 from activating its receptor and thereby modulating the inflammatory cascade. It belongs to the class of IL‑6 receptor antagonists and is administered by intravenous infusion or subcutaneous injection depending on the formulation and indication. Tocilizumab has clinical importance in managing several immune‑mediated inflammatory disorders by reducing cytokine‑driven inflammation and improving disease outcomes when conventional therapies are insufficient or not tolerated. The mechanism of action involves competitive inhibition of IL‑6 binding, which plays a central role in inflammatory responses and acute phase reactions. Tocilizumab’s ability to attenuate IL‑6 signaling has led to its use in chronic conditions like rheumatoid arthritis as well as acute hyperinflammatory states such as cytokine release syndrome. Its development has expanded treatment options for patients with refractory inflammatory diseases and is available in multiple formulations to accommodate different clinical settings.
Background and Date of Approval
Tocilizumab, marketed as Actemra and other biosimilars, underwent development as the first IL‑6 receptor antagonist for human use and demonstrated efficacy in autoimmune and inflammatory diseases in global clinical trials. The United States Food and Drug Administration first approved Actemra (tocilizumab) on January 8, 2010 for adult patients with moderately to severely active rheumatoid arthritis who had an inadequate response to one or more disease‑modifying antirheumatic drugs. Subsequent approvals by the FDA and other regulatory authorities expanded its indications over time to include polyarticular juvenile idiopathic arthritis and systemic juvenile idiopathic arthritis in patients aged two years and older, giant cell arteritis, chimeric antigen receptor T‑cell‑induced severe or life‑threatening cytokine release syndrome on August 30, 2017, and additional inflammatory conditions. Biosimilar versions such as Avtozma (tocilizumab‑anoh) received FDA approval on January 24, 2025 for similar indications, aligning with reference product uses across multiple disease states. The European Medicines Agency and other global authorities have also granted approvals for Actemra and tocilizumab biosimilars across overlapping indications.
Uses
Tocilizumab is approved for the treatment of moderately to severely active rheumatoid arthritis in adult patients who have had an inadequate response to one or more disease‑modifying antirheumatic drugs either as monotherapy or in combination therapy. It is also indicated for polyarticular and systemic juvenile idiopathic arthritis in patients aged two years and older, giant cell arteritis in adults, and severe or life‑threatening cytokine release syndrome associated with chimeric antigen receptor T‑cell therapy in adults and pediatric patients. Some regulatory authorities include additional indications such as systemic sclerosis‑associated interstitial lung disease and coronavirus disease 2019 in specific patient populations when used in conjunction with systemic corticosteroids. Tocilizumab’s indications across these conditions reflect its role in targeting IL‑6 mediated inflammation where conventional therapies have been insufficient or are contraindicated.
Administration
Tocilizumab is administered by healthcare providers either by intravenous infusion or subcutaneous injection depending on the indication, patient weight, and formulation. For adult rheumatoid arthritis, an initial intravenous dose of 4 mg per kilogram every four weeks may be increased to 8 mg per kilogram every four weeks based on clinical response with a maximum of 800 mg per dose. Subcutaneous regimens include fixed doses of 162 mg weekly or every other week contingent upon patient weight and clinical judgement. Younger patients and specific conditions such as cytokine release syndrome may require weight‑based intravenous dosing according to established clinical protocols. Administration schedules are individualized based on the disease being treated, patient response, laboratory parameters, and concomitant therapies, and regular monitoring of clinical and laboratory markers is recommended throughout treatment.
Side Effects
Frequently observed side effects with tocilizumab include upper respiratory tract infections, nasopharyngitis, headache, hypertension, injection site reactions, and elevated liver enzymes. Other commonly reported adverse effects encompass mild to moderate symptoms reflective of immunomodulation and inflammatory changes, which vary among patients and may be manageable under medical supervision. Monitoring is essential to detect changes in laboratory parameters such as liver function tests or blood counts that may accompany therapy.
Warnings
Serious adverse events associated with tocilizumab include severe infections, gastrointestinal perforations, hypersensitivity reactions including anaphylaxis, and hematological abnormalities. Tocilizumab may increase the risk of opportunistic infections and should be used cautiously in patients with pre‑existing infections or risk factors for infection. Contraindications include active, severe infections and hypersensitivity to the drug components. Pregnancy risks should be evaluated by clinicians due to immunomodulatory effects, and treatment interruption is advised in the presence of serious toxicities or intolerable adverse reactions.
Precautions
Baseline assessments prior to initiating tocilizumab include evaluation of infection status, liver enzymes, complete blood counts, and vaccination history. Precautions are warranted in special populations such as patients with hepatic or renal impairment, and live vaccines should be avoided during treatment. Tocilizumab’s inhibition of IL‑6 signaling may restore cytochrome P450 enzyme activity and alter the metabolism of drugs metabolized through these pathways; clinicians should consider potential interactions and monitor therapeutic responses of narrow‑therapeutic‑index drugs. Drug interactions may occur with concomitant immunosuppressive therapies and other biological agents, necessitating careful medication reconciliation and patient education.
Expert Tips
Patient selection for tocilizumab should consider disease severity, prior treatment history, and risk factors for infection or laboratory abnormalities. Baseline testing and regular monitoring strategies include liver function tests, complete blood counts, and inflammatory markers. Counseling points focus on infection risk mitigation, recognizing signs of adverse effects, and adherence to administration schedules. Coordination with combination therapies, particularly conventional disease‑modifying agents, requires careful assessment of cumulative immunosuppressive effects. Handling and infusion considerations involve preparation of the appropriate formulation, weight‑based dosing calculations, and ensuring appropriate facilities for intravenous administration when indicated.
