Trastuzumab
Overview
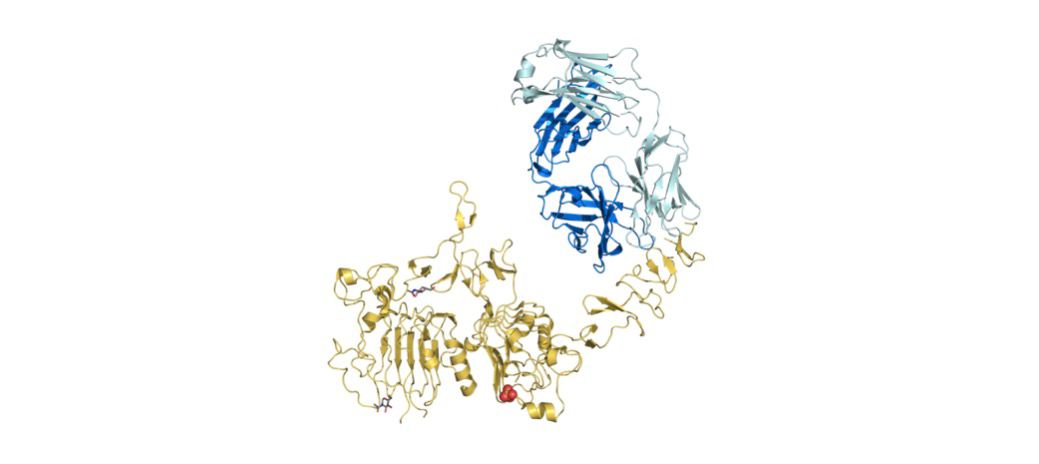
Trastuzumab is a humanized monoclonal antibody that binds to the extracellular domain of the HER2 receptor, blocking HER2-driven signalling and recruiting immune-mediated mechanisms to destroy HER2-expressing tumour cells. It is a core targeted therapy for HER2-positive breast cancer across early, neoadjuvant, adjuvant and metastatic settings and is also indicated for HER2-positive gastric or gastroesophageal junction adenocarcinoma. Trastuzumab is available as an intravenous formulation and as a fixed-dose subcutaneous formulation in certain regions, and it improves progression-free and overall survival when used appropriately with chemotherapy or other HER2-directed agents.
Background and Date of Approval
Trastuzumab was developed to target HER2 (ERBB2), a transmembrane receptor tyrosine kinase overexpressed in a subset of breast and gastric cancers. Initial regulatory approvals established its role in metastatic HER2-positive breast cancer and subsequent trials expanded indications into adjuvant and neoadjuvant therapy and into HER2-positive gastric cancer. Pivotal clinical trials demonstrated significant benefit in disease control and survival when trastuzumab is added to standard chemotherapy. Label warnings include cardiomyopathy, infusion reactions, embryo-fetal toxicity and rare pulmonary toxicity; both intravenous and subcutaneous formulations are described in prescribing information.
Uses
Trastuzumab is indicated for: HER2-positive early-stage breast cancer as part of adjuvant or neoadjuvant therapy; HER2-positive metastatic breast cancer; and HER2-positive metastatic gastric or gastroesophageal junction adenocarcinoma in combination with chemotherapy where appropriate. It is commonly used in combination regimens (for example, with taxanes in breast cancer or platinum plus fluoropyrimidine in gastric cancer) and may be used to downstage disease before surgery. Off-label or investigational uses should be guided by specialist recommendation.
Administration
Trastuzumab is administered intravenously or as a fixed-dose subcutaneous injection (where available) under medical supervision. Common IV schedules: for weekly regimens, an initial loading dose of 4 mg/kg IV followed by 2 mg/kg weekly; for three-weekly regimens, an initial loading dose of 8 mg/kg IV followed by 6 mg/kg every three weeks. In early breast cancer, therapy is typically continued to complete approximately 52 weeks of treatment. The subcutaneous formulation is administered as a fixed dose, typically every three weeks. First infusions are given more slowly (for example, over 90 minutes), and subsequent infusions may be shorter if tolerated. Dose modifications are guided by severity of adverse events and cardiac function assessments per official prescribing guidance.
Side Effects
Common adverse effects include fever and chills during or shortly after infusion, fatigue, nausea, diarrhea, headache, and local injection-site reactions with subcutaneous dosing. Infusion-related symptoms are most frequent with the first dose and often decrease with subsequent administrations. Most side effects are manageable with supportive care and symptomatic treatment.
Warnings
Trastuzumab can cause cardiomyopathy presenting as a decrease in left ventricular ejection fraction and symptomatic congestive heart failure; baseline and periodic cardiac function assessment is recommended. Severe infusion-related or hypersensitivity reactions can occur and require immediate management. Pulmonary toxicity, including interstitial lung disease, has been reported rarely. Use during pregnancy can cause fetal harm; effective contraception is required for patients of childbearing potential during treatment and during the recommended period after the last dose. Concomitant or recent use of anthracyclines increases the risk of cardiac dysfunction and requires careful coordination and monitoring.
Precautions
Confirm HER2 positivity with an approved diagnostic test before initiating trastuzumab. Avoid concurrent use with anthracyclines if possible, due to additive cardiotoxicity; if sequential use is necessary, cardiac function should be monitored closely. Trastuzumab is not metabolized via cytochrome P450 and has minimal pharmacokinetic interactions, but combined use with other immunosuppressive or cytotoxic agents may increase risk of infections and overlapping toxicities. Live vaccines should generally be avoided during and after treatment until immune recovery. Specialist oversight is required for patients with active infections, significant cardiac disease, or prior severe infusion reactions.
Expert Tips
Verify HER2 status (for example via IHC or FISH) before prescribing trastuzumab. Document baseline cardiac function (such as by echocardiogram or MUGA scan) and schedule periodic reassessments during therapy. Consider pausing therapy for significant drops in LVEF according to prescribing guidelines. Counsel patients to report symptoms of heart failure, infusion reactions, pulmonary difficulties, or infection immediately. Prepare the infusion area with resuscitation capability and trained staff. When switching between IV and subcutaneous formulations, ensure correct dosing, administration technique, and scheduling in pharmacy and clinic systems.
