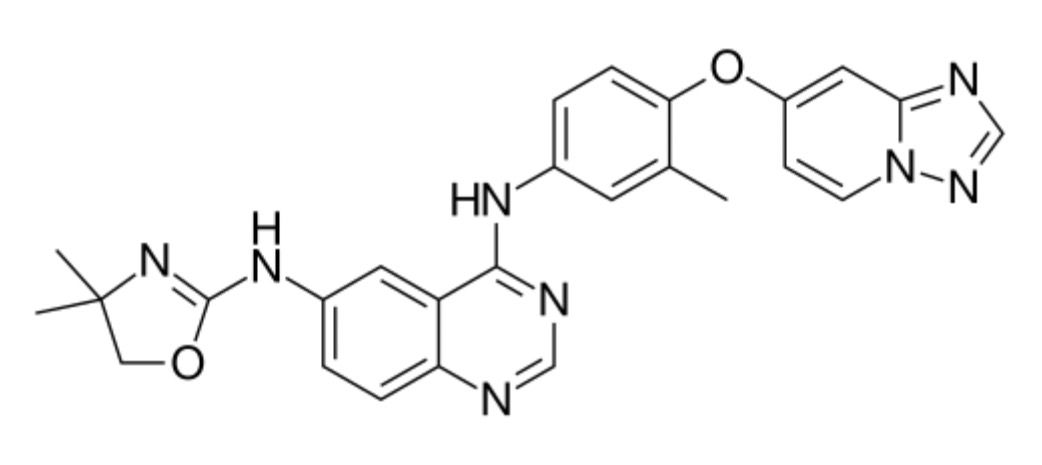
Tucatinib
Overview
Tucatinib is an oral small molecule tyrosine kinase inhibitor specifically targeting the HER2 receptor, used primarily in the treatment of HER2-positive breast cancer. It is designed to inhibit the proliferation of cancer cells that overexpress HER2, a protein involved in aggressive breast tumor growth. Tucatinib is approved for use in combination with other therapies, such as trastuzumab and capecitabine, in patients with advanced or metastatic HER2-positive breast cancer, including those with brain metastases. This targeted therapy offers an important option with a favorable safety profile compared to some other HER2 inhibitors. Monitoring for side effects and periodic clinical evaluation are recommended during treatment.
Background and Date of Approval
Tucatinib was developed to selectively inhibit the tyrosine kinase domain of the HER2 receptor, thereby blocking the downstream signaling pathways that promote cancer cell growth and survival. It differs from earlier HER2-targeted therapies by its increased selectivity, which helps reduce off-target side effects. The drug received accelerated approval by the U.S. Food and Drug Administration (FDA) in 2020 for use in combination therapy for adult patients with advanced unresectable or metastatic HER2-positive breast cancer who have received one or more prior anti-HER2-based regimens. The European Medicines Agency (EMA) also granted approval shortly thereafter. Key clinical trials, including the HER2CLIMB study, demonstrated tucatinib’s efficacy in improving progression-free survival and overall survival, notably in patients with brain metastases.
Uses
Tucatinib is approved for the treatment of adult patients with HER2-positive locally advanced unresectable or metastatic breast cancer who have received at least one prior anti-HER2-based regimen. It is used in combination with trastuzumab and capecitabine. Off-label uses are limited and should be considered only under specialist supervision. Tucatinib is particularly noted for its activity against brain metastases from HER2-positive breast cancer, providing a treatment option for patients with central nervous system involvement. The standard clinical indication emphasizes its role in combination regimens rather than as monotherapy.
Administration
Tucatinib is administered orally, typically as tablets taken twice daily with or without food. The recommended dose is 300 mg per day, divided into two 150 mg doses given approximately 12 hours apart. Dose adjustments may be necessary in patients with severe hepatic impairment. Treatment should continue until disease progression or unacceptable toxicity occurs. Regular clinical monitoring, including liver function tests and assessment of adverse reactions, is advised. Dose modifications may be required for certain adverse effects according to treatment guidelines.
Side Effects
The most commonly reported side effects of tucatinib include diarrhea, palmar-plantar erythrodysesthesia syndrome (hand-foot syndrome), nausea, fatigue, and increased liver enzymes. Diarrhea is generally mild to moderate but may require medical management if severe. Other frequent adverse effects include rash, vomiting, stomatitis, and decreased appetite. Patients are advised to report any severe or persistent symptoms to their healthcare provider promptly for appropriate management.
Warnings
Serious adverse events associated with tucatinib include hepatotoxicity, which may present as elevated liver enzymes or bilirubin levels. Severe diarrhea leading to dehydration is another potential risk. Caution is advised in patients with pre-existing liver impairment. Tucatinib is contraindicated during pregnancy due to potential harm to the fetus and should be used with effective contraception in women of childbearing potential. Hypersensitivity reactions and interstitial lung disease/pneumonitis have been reported rarely. Close monitoring for these conditions is recommended during treatment.
Precautions
Tucatinib is metabolized primarily by the liver enzyme CYP3A4; therefore, concomitant use of strong CYP3A4 inhibitors or inducers may affect tucatinib plasma levels and efficacy. Patients should avoid grapefruit and grapefruit juice during treatment. Caution is warranted when tucatinib is co-administered with other drugs metabolized by CYP3A4. The safety of tucatinib during breastfeeding has not been established. Elderly patients should be monitored carefully for adverse reactions. Vaccination status should be reviewed prior to initiation, and live vaccines should be avoided during treatment.
Expert Tips
When prescribing tucatinib, ensure patients understand the importance of adherence to the twice-daily dosing schedule. Counsel patients on recognizing and managing diarrhea early to prevent dehydration and dose interruptions. Liver function tests should be performed regularly to detect hepatotoxicity early. Coordination with oncology specialists is essential for integrated care, especially when used in combination regimens. Pharmacists should review patients’ medications for potential interactions and educate on avoiding CYP3A4 modifiers. Supportive care measures and patient education can enhance tolerability and treatment outcomes.
