Zanubrutinib
Overview
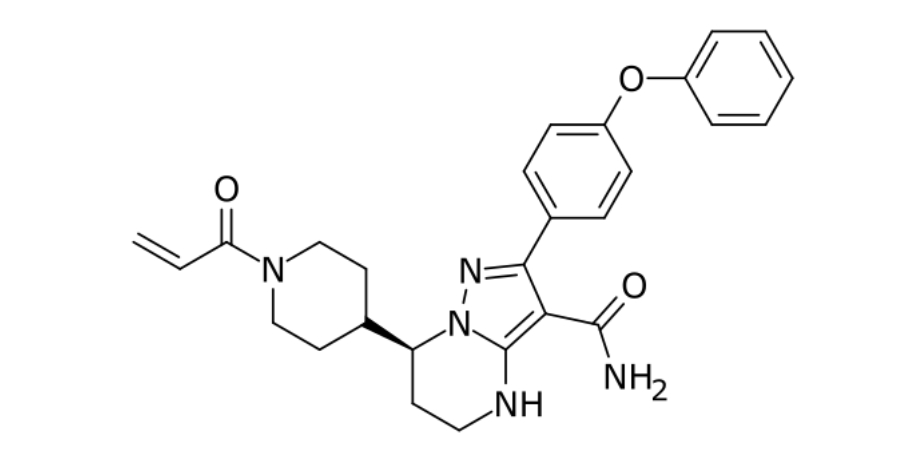
Zanubrutinib is an oral small-molecule targeted therapy that selectively and covalently inhibits Bruton’s tyrosine kinase (BTK), a key signaling molecule involved in the survival, proliferation, and migration of malignant B cells. By blocking BTK, zanubrutinib disrupts B-cell receptor signaling, which leads to reduced tumor cell growth and enhanced apoptosis in B-cell malignancies. Designed as a second-generation BTK inhibitor with high BTK occupancy and minimized off-target effects compared with earlier therapies, zanubrutinib achieves sustained inhibition of malignant B-cell signaling. Its oral administration makes it convenient for long-term treatment, and the drug is used in a range of adult B-cell cancers where BTK-mediated signaling drives disease. Clinical evidence demonstrates meaningful response rates in these cancers, establishing zanubrutinib as an important option in targeted therapy for hematologic malignancies.
Background and Date of Approval
Zanubrutinib, marketed under the brand name Brukinsa, first received regulatory approval in the United States in 2019 for the treatment of adult patients with mantle cell lymphoma who had received at least one prior therapy. Subsequent approvals expanded its indications: in September 2021 for Waldenström’s macroglobulinemia and for relapsed or refractory marginal zone lymphoma after anti-CD20-based therapy, and on January 19, 2023 for chronic lymphocytic leukemia or small lymphocytic lymphoma. Additional marketing authorisations cover its use in other B-cell malignancies including follicular lymphoma in combination with appropriate agents. Regulatory authorities in other regions have likewise authorized zanubrutinib for similar hematologic indications, reflecting broad evidence supporting its benefit in B-cell cancers.
Uses
Zanubrutinib is indicated for the treatment of adult patients with mantle cell lymphoma who have received at least one prior therapy, Waldenström’s macroglobulinemia, chronic lymphocytic leukemia or small lymphocytic lymphoma, and relapsed or refractory marginal zone lymphoma after at least one anti-CD20-based regimen. It is also used in combination with obinutuzumab for adults with follicular lymphoma that has relapsed or is refractory after at least two previous systemic therapies. Its use is tailored to specific B-cell malignancy subtypes, prior treatment history, and patient clinical status.
Administration
Zanubrutinib is administered orally in tablet or capsule form. The recommended dosage for most indications is 160 milligrams taken orally twice daily or 320 milligrams taken orally once daily, and treatment continues until disease progression or unacceptable toxicity. The drug can be taken with or without food at approximately the same times each day. Dose modifications or interruptions may be necessary for adverse reactions or significant toxicities. Baseline and ongoing assessments of hematologic parameters and clinical status help guide safe dosing and continuation of therapy.
Side Effects
Common side effects seen with zanubrutinib include neutropenia, upper respiratory tract infections, decreased platelet count, hemorrhage, rash, musculoskeletal pain, anemia, bruising, diarrhea, pneumonia, and cough. These effects vary in severity and frequency among patients, and supportive care measures alongside clinical monitoring may help manage symptoms during treatment.
Warnings
Serious adverse events associated with zanubrutinib include hemorrhage requiring medical intervention, infections including pneumonia or sepsis, cytopenias such as severe neutropenia or thrombocytopenia, second primary malignancies including non-skin cancers, and cardiac arrhythmias including atrial fibrillation or flutter. Hepatotoxicity and serious skin reactions may also occur. Zanubrutinib is contraindicated in patients with known hypersensitivity to the drug and requires careful monitoring for signs of severe toxicity. Prompt evaluation and management of serious events are essential to minimize harm.
Precautions
Before initiating zanubrutinib therapy, baseline complete blood counts, liver function tests, and cardiac assessment are recommended. Caution is advised in patients with significant cardiovascular disease, bleeding disorders, or severe hepatic impairment. Zanubrutinib is metabolized primarily by hepatic pathways, and co-administration with strong CYP3A inhibitors or inducers may affect drug levels and toxicity risk. Live vaccines should generally be avoided during treatment due to potential immunosuppression. Regular clinical and laboratory monitoring is necessary to identify emerging toxicities and guide therapeutic adjustments.
Expert Tips
Appropriate patient selection for zanubrutinib involves confirming a regulatory-approved indication based on tumor type and prior therapies. Baseline and periodic monitoring of blood counts, liver function, and clinical signs of infection or bleeding are critical to detecting adverse events early. Counsel patients on recognizing symptoms of cytopenias, infections, unusual bruising or bleeding, and cardiac arrhythmias, and educate them on the importance of adherence to dosing schedules. Coordination with multidisciplinary oncology teams facilitates comprehensive management, ensures timely dose adjustments, and enhances supportive care to optimize outcomes and tolerability.
